Tuesday Poster Session
Category: Biliary/Pancreas
P2970 - A Rare Case of Cholangitis Due to Pancreatic Drain Migration After Pancreaticoduodenectomy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Alexandra R. Fiedler, MD
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Alexandra R. Fiedler, MD, Banreet S. Dhindsa, MD, Shailender Singh, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: Pancreaticoduodenectomy, commonly referred to as the Whipple procedure, has significant postoperative morbidity associated. Serious complications include fistula formation, leakage of pancreatic enzymes, and failure of the anastomoses. A pancreatic stent/drain is often placed to bridge the pancreaticoenteric anastomosis and reduce the risk of these complications. Most pancreatic drains placed during a Whipple will spontaneously pass through the small bowel. We present a rare case of cholangitis caused by retrograde pancreatic drain migration to the biliary tree two years after pancreaticoduodenectomy.
Case Description/Methods: An 81-year-old female with history of adenocarcinoma of the distal transverse colon status post resection with late locoregional recurrence of the disease at the proximal duodenum that was surgically resected via classic Whipple procedure presented two years later with fevers, night sweats, and new-onset jaundice. Labs showed a cholestatic pattern of liver enzymes with alkaline phosphatase 1327 u/L, bilirubin 1.2 mg/dL, aspartate aminotransferase (AST) 56 u/l, and alanine transferase (ALT) 41 u/l. Computed tomography demonstrated pneumobilia and pancreatic stent migration to the bile duct area. Antibiotics were started and endoscopic retrograde cholangiopancreatography (ERCP) was performed to retrieve the migrated drain. Patent gastrojejunostomy was visualized along with a normal alimentary limb. From the biliary limb, the previously placed pancreatic duct 5-French drain was seen in the hepaticojejunostomy (HJ) and it was removed intact using a rat-tooth forceps. Biliary cannulation was then performed, and a cholangiogram demonstrated a filling defect in the common hepatic duct. Controlled radial expansion (CRE) dilation was performed with a 6-8 mm balloon up to 7 mm of the HJ anastomosis. Balloon sweeps resulted in the extraction of multiple small stones and sludge. Occlusive cholangiogram was without filling defects. The patient had resolution of her symptoms and has continued to do well three months post-procedure.
Discussion: Migrated stents/drains can serve as a nidus for stone formation and infection that can lead to the development of cholangitis. Although rare, pancreatic drain migration is an important consideration in patients presenting with cholangitis months to years after the Whipple procedure.

Disclosures:
Alexandra R. Fiedler, MD, Banreet S. Dhindsa, MD, Shailender Singh, MD. P2970 - A Rare Case of Cholangitis Due to Pancreatic Drain Migration After Pancreaticoduodenectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Nebraska Medical Center, Omaha, NE
Introduction: Pancreaticoduodenectomy, commonly referred to as the Whipple procedure, has significant postoperative morbidity associated. Serious complications include fistula formation, leakage of pancreatic enzymes, and failure of the anastomoses. A pancreatic stent/drain is often placed to bridge the pancreaticoenteric anastomosis and reduce the risk of these complications. Most pancreatic drains placed during a Whipple will spontaneously pass through the small bowel. We present a rare case of cholangitis caused by retrograde pancreatic drain migration to the biliary tree two years after pancreaticoduodenectomy.
Case Description/Methods: An 81-year-old female with history of adenocarcinoma of the distal transverse colon status post resection with late locoregional recurrence of the disease at the proximal duodenum that was surgically resected via classic Whipple procedure presented two years later with fevers, night sweats, and new-onset jaundice. Labs showed a cholestatic pattern of liver enzymes with alkaline phosphatase 1327 u/L, bilirubin 1.2 mg/dL, aspartate aminotransferase (AST) 56 u/l, and alanine transferase (ALT) 41 u/l. Computed tomography demonstrated pneumobilia and pancreatic stent migration to the bile duct area. Antibiotics were started and endoscopic retrograde cholangiopancreatography (ERCP) was performed to retrieve the migrated drain. Patent gastrojejunostomy was visualized along with a normal alimentary limb. From the biliary limb, the previously placed pancreatic duct 5-French drain was seen in the hepaticojejunostomy (HJ) and it was removed intact using a rat-tooth forceps. Biliary cannulation was then performed, and a cholangiogram demonstrated a filling defect in the common hepatic duct. Controlled radial expansion (CRE) dilation was performed with a 6-8 mm balloon up to 7 mm of the HJ anastomosis. Balloon sweeps resulted in the extraction of multiple small stones and sludge. Occlusive cholangiogram was without filling defects. The patient had resolution of her symptoms and has continued to do well three months post-procedure.
Discussion: Migrated stents/drains can serve as a nidus for stone formation and infection that can lead to the development of cholangitis. Although rare, pancreatic drain migration is an important consideration in patients presenting with cholangitis months to years after the Whipple procedure.

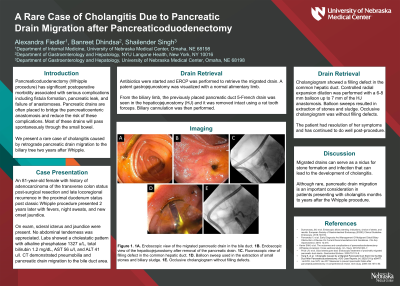
Figure: Figure 1. 1A. Endoscopic view of the migrated pancreatic drain in the bile duct. 1B. Endoscopic view of the choledochojejunostomy after removal of the pancreatic drain. 1C. Fluoroscopic view of filling defect in the common hepatic duct. 1D. Balloon sweep used in the extraction of small stones and biliary sludge. 1E. Occlusive cholangiogram without filling defects.
Disclosures:
Alexandra Fiedler indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Shailender Singh indicated no relevant financial relationships.
Alexandra R. Fiedler, MD, Banreet S. Dhindsa, MD, Shailender Singh, MD. P2970 - A Rare Case of Cholangitis Due to Pancreatic Drain Migration After Pancreaticoduodenectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
