Tuesday Poster Session
Category: Biliary/Pancreas
P2974 - Pancreatic Insulinoma: A Hidden Challenge
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- KM
Karthik Mathialagan, MD
Yale New Haven Health/Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Karthik Mathialagan, MD1, Darin Dolezal, MD, PhD2, Anil Nagar, MD2
1Yale New Haven Health/Bridgeport Hospital, Bridgeport, CT; 2Yale School of Medicine, New Haven, CT
Introduction: Insulinoma is a functional neuroendocrine tumor with an incidence of 1-3 per million population per year. It may be occult, which significantly delays the diagnosis and increases morbidity due to prolonged hypoglycemia. We present a case of occult insulinoma that remained undiagnosed for a year until it was identified on endoscopic ultrasound (EUS).
Case Description/Methods: A healthy 20-year-old presented to the hospital for recurrent fasting and postprandial hypoglycemia for one year. He denied taking sulphonylureas or exogenous insulin. The initial workup demonstrated a normal abdominal CT, MRI, PET scan, and EUS. A presumptive diagnosis of endogenous hyperinsulinism was made and diazoxide was begun. However, symptoms with hypoglycemia began recurring daily. Evaluation revealed HbA1c 4.2%, TSH 4.010mIU/L, glucose 43mg/dl corresponding to C-peptide 7.3ng/ml, proinsulin 1341pmol/L, IGF-1 169ng/ml, IGF-2 624ng/ml, insulin 20.3mcU/ml, glucagon undetectable, insulin autoantibodies < 0.4nU/ml. Octreotide, verapamil, prednisone were begun, and he underwent repeat EUS, which demonstrated a 2 x 1 cm well-defined hypoechoic lobular mass in the pancreatic tail. Fine Needle Aspiration showed small cells with hyperchromatic nuclei with positive immunostaining for ChromoA, synaptophysin, INSM1, consistent with PNET. Rest of the pancreas was normal. He underwent a laparoscopic distal pancreatectomy, following which serum glucose normalized and symptoms resolved. Pathology revealed a WHO grade 2 pT1 N0 well-differentiated neuroendocrine tumor of the pancreatic tail.
Discussion: Insulinomas most commonly present as episodic unprovoked hypoglycemia. Failure of suppression of insulin secretion during hypoglycemia, such as in our patient, is diagnostic of endogenous hyperinsulinism. Initial imaging studies such as CT/MRI are less sensitive if the lesion is small. Pancreatic EUS with FNA is confirmatory, and EUS is the test of choice if cross-sectional imaging is negative with a positivity of 70–95% in experienced centers. The high spatial resolution of EUS allows the detection of small lesions and their precise anatomical localization with higher accuracy for lesions in the pancreatic head. In non-visual samplings, a Selective arterial calcium stimulation test (SACST), combined with hepatic venous sampling, is highly sensitive to detect insulinomas. Once diagnosed, surgical excision is the treatment of choice, but for small (< 1 cm) lesions that cannot be surgically removed, EUS RFA is an emerging treatment.

Disclosures:
Karthik Mathialagan, MD1, Darin Dolezal, MD, PhD2, Anil Nagar, MD2. P2974 - Pancreatic Insulinoma: A Hidden Challenge, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale New Haven Health/Bridgeport Hospital, Bridgeport, CT; 2Yale School of Medicine, New Haven, CT
Introduction: Insulinoma is a functional neuroendocrine tumor with an incidence of 1-3 per million population per year. It may be occult, which significantly delays the diagnosis and increases morbidity due to prolonged hypoglycemia. We present a case of occult insulinoma that remained undiagnosed for a year until it was identified on endoscopic ultrasound (EUS).
Case Description/Methods: A healthy 20-year-old presented to the hospital for recurrent fasting and postprandial hypoglycemia for one year. He denied taking sulphonylureas or exogenous insulin. The initial workup demonstrated a normal abdominal CT, MRI, PET scan, and EUS. A presumptive diagnosis of endogenous hyperinsulinism was made and diazoxide was begun. However, symptoms with hypoglycemia began recurring daily. Evaluation revealed HbA1c 4.2%, TSH 4.010mIU/L, glucose 43mg/dl corresponding to C-peptide 7.3ng/ml, proinsulin 1341pmol/L, IGF-1 169ng/ml, IGF-2 624ng/ml, insulin 20.3mcU/ml, glucagon undetectable, insulin autoantibodies < 0.4nU/ml. Octreotide, verapamil, prednisone were begun, and he underwent repeat EUS, which demonstrated a 2 x 1 cm well-defined hypoechoic lobular mass in the pancreatic tail. Fine Needle Aspiration showed small cells with hyperchromatic nuclei with positive immunostaining for ChromoA, synaptophysin, INSM1, consistent with PNET. Rest of the pancreas was normal. He underwent a laparoscopic distal pancreatectomy, following which serum glucose normalized and symptoms resolved. Pathology revealed a WHO grade 2 pT1 N0 well-differentiated neuroendocrine tumor of the pancreatic tail.
Discussion: Insulinomas most commonly present as episodic unprovoked hypoglycemia. Failure of suppression of insulin secretion during hypoglycemia, such as in our patient, is diagnostic of endogenous hyperinsulinism. Initial imaging studies such as CT/MRI are less sensitive if the lesion is small. Pancreatic EUS with FNA is confirmatory, and EUS is the test of choice if cross-sectional imaging is negative with a positivity of 70–95% in experienced centers. The high spatial resolution of EUS allows the detection of small lesions and their precise anatomical localization with higher accuracy for lesions in the pancreatic head. In non-visual samplings, a Selective arterial calcium stimulation test (SACST), combined with hepatic venous sampling, is highly sensitive to detect insulinomas. Once diagnosed, surgical excision is the treatment of choice, but for small (< 1 cm) lesions that cannot be surgically removed, EUS RFA is an emerging treatment.

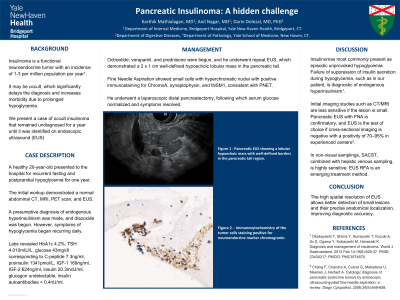
Figure: A - Pancreatic EUS showing a lobular hypoechoic mass with well-defined borders in the pancreatic tail region.
B - Diff-Quik stained FNA smear of the pancreatic neuroendocrine tumor showing cords and nests of tumor cells, admixed with dispersed single tumor cells. (20 x magnification).
C - Immunocytochemistry of the tumor cells staining positive for neuroendocrine marker chromogranin. (40 x magnification).
D - Immunocytochemistry of the tumor cells staining positive for neuroendocrine marker INSM1. (40 x magnification).
B - Diff-Quik stained FNA smear of the pancreatic neuroendocrine tumor showing cords and nests of tumor cells, admixed with dispersed single tumor cells. (20 x magnification).
C - Immunocytochemistry of the tumor cells staining positive for neuroendocrine marker chromogranin. (40 x magnification).
D - Immunocytochemistry of the tumor cells staining positive for neuroendocrine marker INSM1. (40 x magnification).
Disclosures:
Karthik Mathialagan indicated no relevant financial relationships.
Darin Dolezal indicated no relevant financial relationships.
Anil Nagar indicated no relevant financial relationships.
Karthik Mathialagan, MD1, Darin Dolezal, MD, PhD2, Anil Nagar, MD2. P2974 - Pancreatic Insulinoma: A Hidden Challenge, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
