Tuesday Poster Session
Category: Liver
P3975 - Double Trouble: A Rare Case of Hepatosplenic T Cell Lymphoma Masquerading as Giant Cavernous Hepatic Hemangioma With Kasabach-Merritt Phenomenon
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ariella Azimi, DO
Methodist Dallas Medical Center
Dallas, TX
Presenting Author(s)
Ariella Azimi, DO1, Dylan Lopez, MD2, Daniel Gehlbach, DO1, Niels-Jorgen Dyrved, MD1, Mehta Ashwini, DO1
1Methodist Dallas Medical Center, Dallas, TX; 2Methodist Health System of Dallas, Dallas, TX
Introduction: Hepatosplenic T cell lymphoma (HSTCL) is a rare subtype of Peripheral T cell lymphoma that accounts for less than 1% of all Non-Hodgkin’s lymphomas. Histologically, it’s characterized by sinusoidal T cell infiltration of the liver, spleen, and bone marrow and typically presents with B symptoms, cytopenia, and hepatosplenomegaly (HSM). This highly aggressive neoplasm predominantly affects young adult males and is associated with autoimmune conditions, including inflammatory bowel disease. The rapidly progressive and often fatal course of HSTCL creates significant diagnostic and therapeutic challenges for clinicians to overcome. Here we present a case of HSTCL complicated by disseminated intravascular coagulation (DIC) resulting in death.
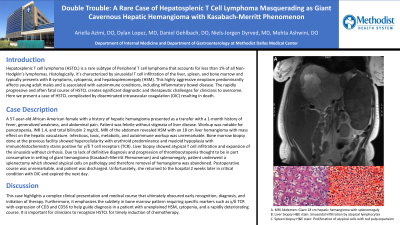
Case Description/Methods: A 57-year-old African American female with a history of hepatic hemangioma presented as a transfer with a 1-month history of fever, generalized weakness, and abdominal pain. Patient was febrile without stigmata of liver disease. Workup was notable for pancytopenia, INR 1.4, and total bilirubin 2 mg/dL. MRI of the abdomen revealed HSM with an 18 cm liver hemangioma with mass effect on the hepatic vasculature. Infectious, toxic, metabolic, and autoimmune workup was unremarkable. Bone marrow biopsy done at the previous facility showed hypercellularity with erythroid predominance and myeloid hypoplasia with immunohistochemistry stains positive for γ/δ T cell receptors (TCR). Liver biopsy showed atypical T cell infiltration and expansion of the sinusoids without cirrhosis. Due to lack of definitive diagnosis and progression of thrombocytopenia thought to be in part consumptive in setting of giant hemangioma (Kasabach-Merritt Phenomenon) and splenomegaly, patient underwent a splenectomy which showed atypical cells on pathology and therefore removal of hemangioma was abandoned. Postoperative course was unremarkable and patient was discharged. Unfortunately, she returned to the hospital 2 weeks later in critical condition with DIC and expired the next day.
Discussion: This case highlights a complex clinical presentation and medical course that ultimately obscured early recognition, diagnosis, and initiation of therapy. Furthermore, it emphasizes the subtlety in bone marrow pattern requiring specific markers such as γ/δ TCR with expression of CD3 and CD56 to help guide diagnosis in a patient with unexplained HSM, cytopenia, and a rapidly deteriorating course. It is important for clinicians to recognize HSTCL for timely induction of chemotherapy.

Disclosures:
Ariella Azimi, DO1, Dylan Lopez, MD2, Daniel Gehlbach, DO1, Niels-Jorgen Dyrved, MD1, Mehta Ashwini, DO1. P3975 - Double Trouble: A Rare Case of Hepatosplenic T Cell Lymphoma Masquerading as Giant Cavernous Hepatic Hemangioma With Kasabach-Merritt Phenomenon, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Methodist Dallas Medical Center, Dallas, TX; 2Methodist Health System of Dallas, Dallas, TX
Introduction: Hepatosplenic T cell lymphoma (HSTCL) is a rare subtype of Peripheral T cell lymphoma that accounts for less than 1% of all Non-Hodgkin’s lymphomas. Histologically, it’s characterized by sinusoidal T cell infiltration of the liver, spleen, and bone marrow and typically presents with B symptoms, cytopenia, and hepatosplenomegaly (HSM). This highly aggressive neoplasm predominantly affects young adult males and is associated with autoimmune conditions, including inflammatory bowel disease. The rapidly progressive and often fatal course of HSTCL creates significant diagnostic and therapeutic challenges for clinicians to overcome. Here we present a case of HSTCL complicated by disseminated intravascular coagulation (DIC) resulting in death.
Case Description/Methods: A 57-year-old African American female with a history of hepatic hemangioma presented as a transfer with a 1-month history of fever, generalized weakness, and abdominal pain. Patient was febrile without stigmata of liver disease. Workup was notable for pancytopenia, INR 1.4, and total bilirubin 2 mg/dL. MRI of the abdomen revealed HSM with an 18 cm liver hemangioma with mass effect on the hepatic vasculature. Infectious, toxic, metabolic, and autoimmune workup was unremarkable. Bone marrow biopsy done at the previous facility showed hypercellularity with erythroid predominance and myeloid hypoplasia with immunohistochemistry stains positive for γ/δ T cell receptors (TCR). Liver biopsy showed atypical T cell infiltration and expansion of the sinusoids without cirrhosis. Due to lack of definitive diagnosis and progression of thrombocytopenia thought to be in part consumptive in setting of giant hemangioma (Kasabach-Merritt Phenomenon) and splenomegaly, patient underwent a splenectomy which showed atypical cells on pathology and therefore removal of hemangioma was abandoned. Postoperative course was unremarkable and patient was discharged. Unfortunately, she returned to the hospital 2 weeks later in critical condition with DIC and expired the next day.
Discussion: This case highlights a complex clinical presentation and medical course that ultimately obscured early recognition, diagnosis, and initiation of therapy. Furthermore, it emphasizes the subtlety in bone marrow pattern requiring specific markers such as γ/δ TCR with expression of CD3 and CD56 to help guide diagnosis in a patient with unexplained HSM, cytopenia, and a rapidly deteriorating course. It is important for clinicians to recognize HSTCL for timely induction of chemotherapy.

Figure: A. MRI Abdomen: Giant 18 cm hepatic hemangioma with splenomegaly
B. Liver biopsy H&E stain: Sinusoidal infiltration by atypical lymphocytes
C. Spleen biopsy H&E stain: Proliferation of atypical cells with red pulp expansion
B. Liver biopsy H&E stain: Sinusoidal infiltration by atypical lymphocytes
C. Spleen biopsy H&E stain: Proliferation of atypical cells with red pulp expansion
Disclosures:
Ariella Azimi indicated no relevant financial relationships.
Dylan Lopez indicated no relevant financial relationships.
Daniel Gehlbach indicated no relevant financial relationships.
Niels-Jorgen Dyrved indicated no relevant financial relationships.
Mehta Ashwini indicated no relevant financial relationships.
Ariella Azimi, DO1, Dylan Lopez, MD2, Daniel Gehlbach, DO1, Niels-Jorgen Dyrved, MD1, Mehta Ashwini, DO1. P3975 - Double Trouble: A Rare Case of Hepatosplenic T Cell Lymphoma Masquerading as Giant Cavernous Hepatic Hemangioma With Kasabach-Merritt Phenomenon, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
