Tuesday Poster Session
Category: Biliary/Pancreas
P2979 - Pancreatic Ascites as a Result of Chronic Pancreatitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Christina Joya
Touro University Nevada
Las Vegas, NV
Presenting Author(s)
Christina Joya, 1, Scott Diamond, DO2, Rebecca Salvo, DO2, Vishvinder Sharma, MD2, Shahid Wahid, MD2
1Touro University Nevada, Las Vegas, NV; 2Valley Hospital Medical Center, Las Vegas, NV
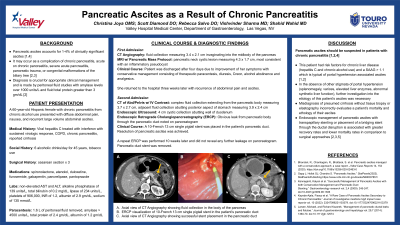
Introduction: Pancreatic ascites accounts for 1-4% of clinically significant ascites and occurs as a result of pancreatic duct (PD) injury.1,2,3 In chronic pancreatitis, PD obstruction from a pseudocyst can create fistula tracts through which pancreatic fluid leaks into the peritoneum.2,3 Peritoneal fluid amylase level >1000 units/L and fluid total protein >3 gm/dL is diagnostic of pancreatic ascites.2 Appropriate diagnosis is crucial to ensure proper management.
Case Description/Methods: A 60-year-old female with treated hepatitis C, chronic alcoholism (6 drinks/day for 45 years) with chronic pancreatitis was admitted to the hospital with diffuse abdominal pain and nausea. She had previously been prescribed spironolactone for ascites and was told she had cirrhosis. Labs revealed non-elevated AST and ALT, ALP 139 u/L, total bilirubin 0.2 mg/dL, lipase 234 u/L, platelets 906k, INR 1.2, albumin 2.9 gm/dL, sodium 135 mmol/L.
An abdominal CT revealed large volume ascites with a fatty liver and a 3.4 x 2.1cm pancreatic pseudocyst. The spleen size was normal. No varices were noted. Patent portal and hepatic vasculature were seen with duplex ultrasound. A diagnostic and therapeutic paracentesis with fluid studies revealed amylase > 4500 units/L, total protein of 2.4 gm/dL, albumin of 1.2 gm/dL, and serum albumin ascites gradient of 1.7 g/dL. This was consistent with pancreatic ascites. Her symptoms resolved with conservative treatment after 4 days and she was discharged.
Three weeks later she returned with recurrent ascites. CT of the abdomen revealed an enlarging pseudocyst. Endoscopic Retrograde Cholangiopancreatography (ERCP) with pancreatogram revealed a leak from the pancreatic body through the PD. A 10-French 13 cm single pigtail PD stent was placed. 10 weeks later, she had no further recurrence of her ascites and an ERCP confirmed resolution of her pancreatic leak. The stent was removed.
Discussion: Ascitic amylase levels are not routinely checked however the absence of other stigmata of portal hypertension prompted further investigation of this patient’s ascites despite her risk factors for chronic liver disease. Pancreatic etiology of ascites must be suspected in patients with chronic pancreatitis as the management differs from other causes of ascites. The consequences of misdiagnosis would prove typical considerations for refractory ascites such as aggressive diuresis or a TIPS ineffective and potentially harmful. Additionally, the appropriate management with stenting would not have been considered.
Disclosures:
Christina Joya, 1, Scott Diamond, DO2, Rebecca Salvo, DO2, Vishvinder Sharma, MD2, Shahid Wahid, MD2. P2979 - Pancreatic Ascites as a Result of Chronic Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Touro University Nevada, Las Vegas, NV; 2Valley Hospital Medical Center, Las Vegas, NV
Introduction: Pancreatic ascites accounts for 1-4% of clinically significant ascites and occurs as a result of pancreatic duct (PD) injury.1,2,3 In chronic pancreatitis, PD obstruction from a pseudocyst can create fistula tracts through which pancreatic fluid leaks into the peritoneum.2,3 Peritoneal fluid amylase level >1000 units/L and fluid total protein >3 gm/dL is diagnostic of pancreatic ascites.2 Appropriate diagnosis is crucial to ensure proper management.
Case Description/Methods: A 60-year-old female with treated hepatitis C, chronic alcoholism (6 drinks/day for 45 years) with chronic pancreatitis was admitted to the hospital with diffuse abdominal pain and nausea. She had previously been prescribed spironolactone for ascites and was told she had cirrhosis. Labs revealed non-elevated AST and ALT, ALP 139 u/L, total bilirubin 0.2 mg/dL, lipase 234 u/L, platelets 906k, INR 1.2, albumin 2.9 gm/dL, sodium 135 mmol/L.
An abdominal CT revealed large volume ascites with a fatty liver and a 3.4 x 2.1cm pancreatic pseudocyst. The spleen size was normal. No varices were noted. Patent portal and hepatic vasculature were seen with duplex ultrasound. A diagnostic and therapeutic paracentesis with fluid studies revealed amylase > 4500 units/L, total protein of 2.4 gm/dL, albumin of 1.2 gm/dL, and serum albumin ascites gradient of 1.7 g/dL. This was consistent with pancreatic ascites. Her symptoms resolved with conservative treatment after 4 days and she was discharged.
Three weeks later she returned with recurrent ascites. CT of the abdomen revealed an enlarging pseudocyst. Endoscopic Retrograde Cholangiopancreatography (ERCP) with pancreatogram revealed a leak from the pancreatic body through the PD. A 10-French 13 cm single pigtail PD stent was placed. 10 weeks later, she had no further recurrence of her ascites and an ERCP confirmed resolution of her pancreatic leak. The stent was removed.
Discussion: Ascitic amylase levels are not routinely checked however the absence of other stigmata of portal hypertension prompted further investigation of this patient’s ascites despite her risk factors for chronic liver disease. Pancreatic etiology of ascites must be suspected in patients with chronic pancreatitis as the management differs from other causes of ascites. The consequences of misdiagnosis would prove typical considerations for refractory ascites such as aggressive diuresis or a TIPS ineffective and potentially harmful. Additionally, the appropriate management with stenting would not have been considered.
Disclosures:
Christina Joya indicated no relevant financial relationships.
Scott Diamond indicated no relevant financial relationships.
Rebecca Salvo indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Shahid Wahid indicated no relevant financial relationships.
Christina Joya, 1, Scott Diamond, DO2, Rebecca Salvo, DO2, Vishvinder Sharma, MD2, Shahid Wahid, MD2. P2979 - Pancreatic Ascites as a Result of Chronic Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

