Tuesday Poster Session
Category: Biliary/Pancreas
P2982 - A Rare Case of Bilateral Pancreatic-Pleural Fistula Mimicking Esophageal Cancer
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Raj Shah, MD
University of Central Florida HCA Healthcare GME
Kissimmee, FL
Presenting Author(s)
Raj Shah, MD1, Feras Al-Moussally, MD1, Natalia Tejada, MD2, Richard Henriquez, MD3, Silvio W. de Melo Jr., MD, FACG4
1University of Central Florida HCA Healthcare GME, Kissimmee, FL; 2University of Central Florida College of Medicine, Orlando, FL; 3Orlando VA Medical Center and UCF/HCA Greater Orlando, St. Cloud, FL; 4Orlando VA Healthcare System, Orlando, FL
Introduction: Pancreaticopleural fistula (PPF) is a rare complication of chronic complication with a < 1% incidence rate. It typically presents as a left massive pleural effusion with thoracic symptoms like shortness of breath, orthopnea, chest pain and cough. We present a rare case of PPF extending into the bilateral pleural space initially being worked up for esophageal cancer after imaging studies suggested malignancy.
Case Description/Methods: A 58-year-old male presented six months after acute pancreatitis with one week of dysphagia. CT scan showed bilateral pleural effusions with a mass at the gastroesophageal junction and thickening of the distal thoracic esophagus consistent with malignancy. Esophagogastroduodenoscopy with biopsy was negative for malignancy. Positron emission tomography scan was unremarkable.
Two months later, he presented with dyspnea and a large left pleural effusion. 1250CC fluid was drained with no evidence of malignant cells and infection. The patient was discharged but returned due to recurrent effusion requiring continuous drainage. Fluid analysis was negative for malignancy. Endoscopic ultrasound for esophageal mass showed fluid tract extending from the tail of pancreas into bilateral pleural space through the esophageal hiatus, consistent with PPF. It was confirmed on MRI and CT. Pleural fluid amylase and lipase were significantly elevated. The patient was started on octreotide and underwent pancreatic stent placement. A follow-up cystogastrostomy was performed and the pancreatic stent was removed without further recurrence of the fluid collections.
Discussion: PPF is usually associated with chronic pancreatitis from alcohol use. It is thought to be due to a direct pancreatic duct leak or a leak from an incompletely formed or ruptured pseudocyst. A pleural fluid analysis with positive amylase, lipase and albumin is imperative but nonspecific. Endoscopic retrograde cholangiopancreatography or magnetic resonance cholangiopancreatography can be useful tools for demonstrating the fistulous pathway.
Diagnosis is often delayed and overlooked because of nonspecific presentation, with some reports ranging from 12 to 49 days. In our case, it mimicked esophageal cancer with recurrent malignant pleural effusion. However, after readmissions, the patient underwent EUS showing PPF that was later confirmed on MRI. Early suspicion in a known case of pancreatitis is encouraged for timely workup and management.

Disclosures:
Raj Shah, MD1, Feras Al-Moussally, MD1, Natalia Tejada, MD2, Richard Henriquez, MD3, Silvio W. de Melo Jr., MD, FACG4. P2982 - A Rare Case of Bilateral Pancreatic-Pleural Fistula Mimicking Esophageal Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Central Florida HCA Healthcare GME, Kissimmee, FL; 2University of Central Florida College of Medicine, Orlando, FL; 3Orlando VA Medical Center and UCF/HCA Greater Orlando, St. Cloud, FL; 4Orlando VA Healthcare System, Orlando, FL
Introduction: Pancreaticopleural fistula (PPF) is a rare complication of chronic complication with a < 1% incidence rate. It typically presents as a left massive pleural effusion with thoracic symptoms like shortness of breath, orthopnea, chest pain and cough. We present a rare case of PPF extending into the bilateral pleural space initially being worked up for esophageal cancer after imaging studies suggested malignancy.
Case Description/Methods: A 58-year-old male presented six months after acute pancreatitis with one week of dysphagia. CT scan showed bilateral pleural effusions with a mass at the gastroesophageal junction and thickening of the distal thoracic esophagus consistent with malignancy. Esophagogastroduodenoscopy with biopsy was negative for malignancy. Positron emission tomography scan was unremarkable.
Two months later, he presented with dyspnea and a large left pleural effusion. 1250CC fluid was drained with no evidence of malignant cells and infection. The patient was discharged but returned due to recurrent effusion requiring continuous drainage. Fluid analysis was negative for malignancy. Endoscopic ultrasound for esophageal mass showed fluid tract extending from the tail of pancreas into bilateral pleural space through the esophageal hiatus, consistent with PPF. It was confirmed on MRI and CT. Pleural fluid amylase and lipase were significantly elevated. The patient was started on octreotide and underwent pancreatic stent placement. A follow-up cystogastrostomy was performed and the pancreatic stent was removed without further recurrence of the fluid collections.
Discussion: PPF is usually associated with chronic pancreatitis from alcohol use. It is thought to be due to a direct pancreatic duct leak or a leak from an incompletely formed or ruptured pseudocyst. A pleural fluid analysis with positive amylase, lipase and albumin is imperative but nonspecific. Endoscopic retrograde cholangiopancreatography or magnetic resonance cholangiopancreatography can be useful tools for demonstrating the fistulous pathway.
Diagnosis is often delayed and overlooked because of nonspecific presentation, with some reports ranging from 12 to 49 days. In our case, it mimicked esophageal cancer with recurrent malignant pleural effusion. However, after readmissions, the patient underwent EUS showing PPF that was later confirmed on MRI. Early suspicion in a known case of pancreatitis is encouraged for timely workup and management.

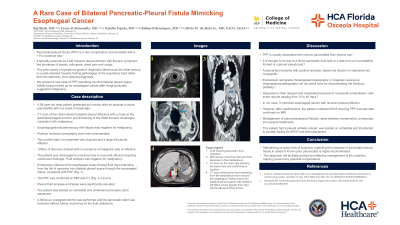
Figure: CT scan showing the tract extending from the mediastinum from around the esophagus (Yellow arrow) into bilateral pleural spaces with bilateral left (Blue arrow) greater than right pleural effusions (Red arrow).
Disclosures:
Raj Shah indicated no relevant financial relationships.
Feras Al-Moussally indicated no relevant financial relationships.
Natalia Tejada indicated no relevant financial relationships.
Richard Henriquez indicated no relevant financial relationships.
Silvio W. de Melo Jr. indicated no relevant financial relationships.
Raj Shah, MD1, Feras Al-Moussally, MD1, Natalia Tejada, MD2, Richard Henriquez, MD3, Silvio W. de Melo Jr., MD, FACG4. P2982 - A Rare Case of Bilateral Pancreatic-Pleural Fistula Mimicking Esophageal Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

