Tuesday Poster Session
Category: Biliary/Pancreas
P2985 - From Pain to Drain: Acute Obstructive Suppurative Pancreatic Ductitis in Chronic Pancreatitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ryan L. Santos, DO
Brooke Army Medical Center
San Antonio, Texas
Presenting Author(s)
Ryan L. Santos, DO, Cyrus Veryl. Edelson, MD, Seth Dukes, MD
Brooke Army Medical Center, San Antonio, TX
Introduction: 60-year-old male with acute-on-chronic pancreatitis secondary to alcohol, who presented for ERCP demonstrating recurrent pancreatitis with sepsis. We highlight this rare case of acute obstructive suppurative pancreatic ductitis (AOSPD) and the need to consider it in the differential of patients with chronic pancreatitis.
Case Description/Methods: A 60yoM with a history of chronic pancreatitis secondary to alcohol, complicated by pancreatic duct stricture and serial ERCPs for stent placement, presents with worsening epigastric abdominal pain with radiation to the back, and intermittent fevers up to 101.3F. Previous attempts to manage his pain include narcotics, TCAs and celiac plexus block with intermittent resolution. CT abdomen with contrast demonstrated peripancreatic inflammatory changes without any evidence of discrete fluid collections, lesions, or necrosis.
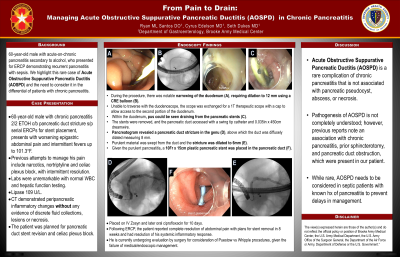
The patient was planned for pancreatic duct stent revision and celiac plexus block. During the procedure, there was notable narrowing of the duodenum, requiring dilation to 12 mm using a CRE balloon. Unable to traverse with the duodenoscope, the scope was exchanged for a 1T therapeutic scope with cap to allow access to the second portion of the duodenum. Within the duodenum, pus could be seen draining from the pancreatic stents. The stents were removed, and the pancreatic duct accessed with a swing tip catheter and 0.035in x 260cm dreamwire. Pancreatogram revealed a pancreatic duct stricture in the genu, above which the duct was diffusely dilated measuring 8 mm. Purulent material was swept from the duct and the stricture was dilated to 8mm. Given the purulent pancreatitis, a 10 Fr by 15 cm plastic pancreatic stent was placed in the pancreatic duct. He was then placed on Zosyn and later ciprofloxacin for 10 days.
Following ERCP, the patient reported complete resolution of pain and systemic inflammatory response. He is currently undergoing evaluation by surgery for consideration of Puestow vs Whipple procedures, given the failure of medical/endoscopic management.
Discussion: AOSPD is a rare complication of chronic pancreatitis that is not associated with pancreatic pseudocyst, abscess or necrosis. The pathogenesis of AOSPD is not completely understood; however, previous reports do note an association with chronic pancreatitis, prior sphincterotomy, and pancreatic duct obstruction, which were present in our patient. While rare, AOSPD needs to be considered in septic patients with known hx of pancreatitis to prevent delays in management.

Disclosures:
Ryan L. Santos, DO, Cyrus Veryl. Edelson, MD, Seth Dukes, MD. P2985 - From Pain to Drain: Acute Obstructive Suppurative Pancreatic Ductitis in Chronic Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Brooke Army Medical Center, San Antonio, TX
Introduction: 60-year-old male with acute-on-chronic pancreatitis secondary to alcohol, who presented for ERCP demonstrating recurrent pancreatitis with sepsis. We highlight this rare case of acute obstructive suppurative pancreatic ductitis (AOSPD) and the need to consider it in the differential of patients with chronic pancreatitis.
Case Description/Methods: A 60yoM with a history of chronic pancreatitis secondary to alcohol, complicated by pancreatic duct stricture and serial ERCPs for stent placement, presents with worsening epigastric abdominal pain with radiation to the back, and intermittent fevers up to 101.3F. Previous attempts to manage his pain include narcotics, TCAs and celiac plexus block with intermittent resolution. CT abdomen with contrast demonstrated peripancreatic inflammatory changes without any evidence of discrete fluid collections, lesions, or necrosis.
The patient was planned for pancreatic duct stent revision and celiac plexus block. During the procedure, there was notable narrowing of the duodenum, requiring dilation to 12 mm using a CRE balloon. Unable to traverse with the duodenoscope, the scope was exchanged for a 1T therapeutic scope with cap to allow access to the second portion of the duodenum. Within the duodenum, pus could be seen draining from the pancreatic stents. The stents were removed, and the pancreatic duct accessed with a swing tip catheter and 0.035in x 260cm dreamwire. Pancreatogram revealed a pancreatic duct stricture in the genu, above which the duct was diffusely dilated measuring 8 mm. Purulent material was swept from the duct and the stricture was dilated to 8mm. Given the purulent pancreatitis, a 10 Fr by 15 cm plastic pancreatic stent was placed in the pancreatic duct. He was then placed on Zosyn and later ciprofloxacin for 10 days.
Following ERCP, the patient reported complete resolution of pain and systemic inflammatory response. He is currently undergoing evaluation by surgery for consideration of Puestow vs Whipple procedures, given the failure of medical/endoscopic management.
Discussion: AOSPD is a rare complication of chronic pancreatitis that is not associated with pancreatic pseudocyst, abscess or necrosis. The pathogenesis of AOSPD is not completely understood; however, previous reports do note an association with chronic pancreatitis, prior sphincterotomy, and pancreatic duct obstruction, which were present in our patient. While rare, AOSPD needs to be considered in septic patients with known hx of pancreatitis to prevent delays in management.

Figure: Pancreatic stents draining pus.
Disclosures:
Ryan Santos indicated no relevant financial relationships.
Cyrus Edelson indicated no relevant financial relationships.
Seth Dukes indicated no relevant financial relationships.
Ryan L. Santos, DO, Cyrus Veryl. Edelson, MD, Seth Dukes, MD. P2985 - From Pain to Drain: Acute Obstructive Suppurative Pancreatic Ductitis in Chronic Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
