Tuesday Poster Session
Category: Biliary/Pancreas
P2987 - Acute Necrotizing Pancreatitis: Who Is the Real Culprit?
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Samdish Sethi, MD
Yale New Haven Health/Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Samdish Sethi, MD, Karthik Mathialagan, MD
Yale New Haven Health/Bridgeport Hospital, Bridgeport, CT
Introduction: Acute pancreatitis has been the leading cause of GI-related hospitalization in the US lately. Alcohol and gallstones have been implicated as the major cause of acute pancreatitis while drug induced pancreatitis (DIP) once considered a rare entity, has been increasingly reported in recent years and accounts for 0.1% - 2% of these cases. We present a case of acute necrotizing pancreatitis caused by Trimethoprim-Sulfamethoxazole.
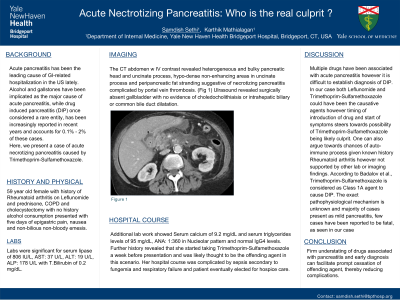
Case Description/Methods: 59 year old female with PMHx of Rheumatoid arthritis on Leflunomide and prednisone, COPD and cholecystectomy with no history of alcohol consumption presented with five days of epigastric pain, nausea and non-bilious non-bloody emesis. Labs were significant for Lipase of 806 IU/L, AST: 37 U/L, ALT: 19 U/L, ALP: 178 U/L and T.Bilirubin of 0.2 mg/dL. Serum calcium was 9.2 mg/dL and triglycerides level was 95 mg/dL. CT abdomen w IV contrast revealed heterogeneous, bulky pancreatic head and uncinate process, hypo-dense non-enhancing areas in uncinate process and peri-pancreatic fat stranding suggestive of necrotizing pancreatitis complicated by portal vein thrombosis. Ultrasound revealed surgically absent gallbladder with no evidence of choledocholithiaisis or intrahepatic biliary or common bile duct dilatation. Additional labs showed ANA: 1:360 in Nucleolar pattern and normal IgG4 levels. History revealed that she started taking Trimethoprim-Sulfamethoxazole for UTI a week before presentation and was likely thought to be the offending agent. Her hospital course was complicated by sepsis secondary to fungemia and respiratory failure and patient eventually elected for hospice care.
Discussion: Multiple drugs have been associated with acute pancreatitis however it is difficult to establish diagnosis of DIP. In our case both Leflunomide and Trimethoprim-Sulfamethoxazole could have been causative agents however timing of introduction of drug and start of symptoms steers towards possibility of later being the likely culprit. One can also argue for chances of auto-immune process given history of Rheumatoid arthritis however was not supported by other lab or imaging findings. According to Badalov et al., Trimethoprim-Sulfamethoxazole is considered as Class 1A agent to cause DIP. The exact pathophysiological mechanism is unknown with majority cases being mild and few fatal cases have been reported. Firm understating of drugs associated with pancreatitis and early diagnosis can facilitate prompt cessation of offending agent, thereby reducing complications.

Disclosures:
Samdish Sethi, MD, Karthik Mathialagan, MD. P2987 - Acute Necrotizing Pancreatitis: Who Is the Real Culprit?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Yale New Haven Health/Bridgeport Hospital, Bridgeport, CT
Introduction: Acute pancreatitis has been the leading cause of GI-related hospitalization in the US lately. Alcohol and gallstones have been implicated as the major cause of acute pancreatitis while drug induced pancreatitis (DIP) once considered a rare entity, has been increasingly reported in recent years and accounts for 0.1% - 2% of these cases. We present a case of acute necrotizing pancreatitis caused by Trimethoprim-Sulfamethoxazole.
Case Description/Methods: 59 year old female with PMHx of Rheumatoid arthritis on Leflunomide and prednisone, COPD and cholecystectomy with no history of alcohol consumption presented with five days of epigastric pain, nausea and non-bilious non-bloody emesis. Labs were significant for Lipase of 806 IU/L, AST: 37 U/L, ALT: 19 U/L, ALP: 178 U/L and T.Bilirubin of 0.2 mg/dL. Serum calcium was 9.2 mg/dL and triglycerides level was 95 mg/dL. CT abdomen w IV contrast revealed heterogeneous, bulky pancreatic head and uncinate process, hypo-dense non-enhancing areas in uncinate process and peri-pancreatic fat stranding suggestive of necrotizing pancreatitis complicated by portal vein thrombosis. Ultrasound revealed surgically absent gallbladder with no evidence of choledocholithiaisis or intrahepatic biliary or common bile duct dilatation. Additional labs showed ANA: 1:360 in Nucleolar pattern and normal IgG4 levels. History revealed that she started taking Trimethoprim-Sulfamethoxazole for UTI a week before presentation and was likely thought to be the offending agent. Her hospital course was complicated by sepsis secondary to fungemia and respiratory failure and patient eventually elected for hospice care.
Discussion: Multiple drugs have been associated with acute pancreatitis however it is difficult to establish diagnosis of DIP. In our case both Leflunomide and Trimethoprim-Sulfamethoxazole could have been causative agents however timing of introduction of drug and start of symptoms steers towards possibility of later being the likely culprit. One can also argue for chances of auto-immune process given history of Rheumatoid arthritis however was not supported by other lab or imaging findings. According to Badalov et al., Trimethoprim-Sulfamethoxazole is considered as Class 1A agent to cause DIP. The exact pathophysiological mechanism is unknown with majority cases being mild and few fatal cases have been reported. Firm understating of drugs associated with pancreatitis and early diagnosis can facilitate prompt cessation of offending agent, thereby reducing complications.

Figure: CT abdomen with IV contrast : Necrotizing pancreatitis
Disclosures:
Samdish Sethi indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Samdish Sethi, MD, Karthik Mathialagan, MD. P2987 - Acute Necrotizing Pancreatitis: Who Is the Real Culprit?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
