Tuesday Poster Session
Category: Liver
P3990 - Primary Hepatic Burkitt Lymphoma: A Histological Highlight
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sara Yacyshyn, MD
Wright State University Boonshoft School of Medicine
Dayton, OH
Presenting Author(s)
Matthew Silverman, MD1, Bradley Karmo, 2, Fadi Odish, MD1, Sara Yacyshyn, MD1, Rebecca Balaj, MD3, Drew Triplett, DO4
1Wright State University Boonshoft School of Medicine, Dayton, OH; 2Michigan State University College of Osteopathic Medicine, East Lansing, MI; 3Miami Valley Hospital, Dayton, OH; 4Dayton Gastroenterology, Dayton, OH
Introduction: Burkitt lymphoma (BL) is an aggressive B-cell lymphoma with the gastrointestinal tract as the most common extra nodal site. Primary hepatic Burkitt lymphoma (PHBL) is an exceedingly rare subtype, accounting for < 0.5% of cases. In this report, we describe a case of primary hepatic Burkitt lymphoma.
Case Description/Methods: A 47 year-old man with fatty liver disease presented to the hospital with a 3-month history of constant abdominal pain, early satiety, and weight loss beginning at home in Iraq.
He reported nausea but denied emesis, diarrhea, constipation, jaundice, or signs of blood loss. He denied tobacco, alcohol or drug use, and was in a monogamous relationship with his wife. Exam was negative for fluid wave, jaundice, rebound, and guarding. Serologic workup was notable for mild hepatocellular and cholestatic patterns without leukocytosis or eosinophilia. Viral hepatitis serologies and cancer markers were negative.
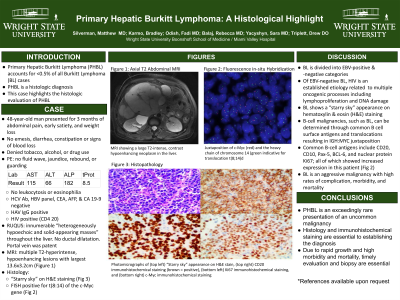
Ultrasound of the liver showed innumerable masses in the liver with a patent portal vein and no biliary dilatation. MRI revealed multiple T2-hyperintense, hypoenhancing lesions with the largest measuring 13 x 3cm (Figure 1a). The gallbladder was normal.
Liver biopsy and subsequent histology showed numerous lymphocytes with macrophage tangles (Figure 1b). Fluorescence in-situ hybridization displayed a translocation between chromosomes 8 and 14 (t(8;14)) (Figure 1c), establishing a diagnosis of primary hepatic Burkitt lymphoma.
Despite multiple complications, he responded well to aggressive chemotherapy regimen with normalization of transaminases and vast reduction in the liver lesions.
Discussion: Histological evaluation is key to diagnosis and basic H&E staining displays the classic “starry-sky” appearance as portrayed in this case (Figure 1b). As a B-cell tumor, BL tissue samples can be analyzed for B-cell surface antigens and the IGH:MYC (Figure 1c) juxtaposition via chromosomal translocation as displayed above. Given the well-defined surface markers and known translocation, immunostaining and fluorescence in-situ hybridization are apt diagnostic modalities for diagnosis of BL.
Due to rapid growth, a large tumor burden is often present at the time of diagnosis. High-intensity chemotherapy regimens are required with cytotoxic and infectious diseases often complicating therapy. These facts with the commonly ambiguous clinical presentation highlight the importance of rapid imaging and histologic evaluation in optimizing outcomes in PHBL.

Disclosures:
Matthew Silverman, MD1, Bradley Karmo, 2, Fadi Odish, MD1, Sara Yacyshyn, MD1, Rebecca Balaj, MD3, Drew Triplett, DO4. P3990 - Primary Hepatic Burkitt Lymphoma: A Histological Highlight, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wright State University Boonshoft School of Medicine, Dayton, OH; 2Michigan State University College of Osteopathic Medicine, East Lansing, MI; 3Miami Valley Hospital, Dayton, OH; 4Dayton Gastroenterology, Dayton, OH
Introduction: Burkitt lymphoma (BL) is an aggressive B-cell lymphoma with the gastrointestinal tract as the most common extra nodal site. Primary hepatic Burkitt lymphoma (PHBL) is an exceedingly rare subtype, accounting for < 0.5% of cases. In this report, we describe a case of primary hepatic Burkitt lymphoma.
Case Description/Methods: A 47 year-old man with fatty liver disease presented to the hospital with a 3-month history of constant abdominal pain, early satiety, and weight loss beginning at home in Iraq.
He reported nausea but denied emesis, diarrhea, constipation, jaundice, or signs of blood loss. He denied tobacco, alcohol or drug use, and was in a monogamous relationship with his wife. Exam was negative for fluid wave, jaundice, rebound, and guarding. Serologic workup was notable for mild hepatocellular and cholestatic patterns without leukocytosis or eosinophilia. Viral hepatitis serologies and cancer markers were negative.
Ultrasound of the liver showed innumerable masses in the liver with a patent portal vein and no biliary dilatation. MRI revealed multiple T2-hyperintense, hypoenhancing lesions with the largest measuring 13 x 3cm (Figure 1a). The gallbladder was normal.
Liver biopsy and subsequent histology showed numerous lymphocytes with macrophage tangles (Figure 1b). Fluorescence in-situ hybridization displayed a translocation between chromosomes 8 and 14 (t(8;14)) (Figure 1c), establishing a diagnosis of primary hepatic Burkitt lymphoma.
Despite multiple complications, he responded well to aggressive chemotherapy regimen with normalization of transaminases and vast reduction in the liver lesions.
Discussion: Histological evaluation is key to diagnosis and basic H&E staining displays the classic “starry-sky” appearance as portrayed in this case (Figure 1b). As a B-cell tumor, BL tissue samples can be analyzed for B-cell surface antigens and the IGH:MYC (Figure 1c) juxtaposition via chromosomal translocation as displayed above. Given the well-defined surface markers and known translocation, immunostaining and fluorescence in-situ hybridization are apt diagnostic modalities for diagnosis of BL.
Due to rapid growth, a large tumor burden is often present at the time of diagnosis. High-intensity chemotherapy regimens are required with cytotoxic and infectious diseases often complicating therapy. These facts with the commonly ambiguous clinical presentation highlight the importance of rapid imaging and histologic evaluation in optimizing outcomes in PHBL.

Figure: A. MRI showing a large T2 hyper-intense, contrast-hypoenhancing neoplasm in the liver;
B. Hematoxylin & eosin (H&E) staining showing basophilic lymphocytes surrounded by macrophages with tangles with the characteristic "starry-sky" appearance;
C. Juxtaposition of c-Myc (red) and the heavy chain of chromosome 14 (green) indicative of the characteristic translocation t(8;14).
B. Hematoxylin & eosin (H&E) staining showing basophilic lymphocytes surrounded by macrophages with tangles with the characteristic "starry-sky" appearance;
C. Juxtaposition of c-Myc (red) and the heavy chain of chromosome 14 (green) indicative of the characteristic translocation t(8;14).
Disclosures:
Matthew Silverman indicated no relevant financial relationships.
Bradley Karmo indicated no relevant financial relationships.
Fadi Odish indicated no relevant financial relationships.
Sara Yacyshyn indicated no relevant financial relationships.
Rebecca Balaj indicated no relevant financial relationships.
Drew Triplett indicated no relevant financial relationships.
Matthew Silverman, MD1, Bradley Karmo, 2, Fadi Odish, MD1, Sara Yacyshyn, MD1, Rebecca Balaj, MD3, Drew Triplett, DO4. P3990 - Primary Hepatic Burkitt Lymphoma: A Histological Highlight, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
