Tuesday Poster Session
Category: Biliary/Pancreas
P2990 - A Rare Presentation of Cholecystocolonic Fistula
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Anuroop Yekula, MD
Saint Vincent Hospital
Worcester, MA
Presenting Author(s)
Anuroop Yekula, MD1, Mythri Subramaniam, MD2, Anna Leszczynksi, MD2
1Saint Vincent Hospital, Worcester, MA; 2Lahey Hospital, Burlington, MA
Introduction: Cholecystoenteric fistula is a rare disease that is usually seen with biliary pathologies. Cholecystocolonic fistulas (CCF) comprise at least 10-20% of cholecystoenteric fistulas. It is most commonly a result of biliary disease, especially cholelithiasis but also reported to be from abdominal trauma, IBD, and malignancy of the pancreaticobiliary system.
Here, we present a rare case of CCF from an occult luminal intestinal malignancy.
Case Description/Methods: A 45-year-old male with a medical history of type 1 diabetes initially presents with fatigue, nausea, and decreased appetite. His physical exam was unrevealing, but he was noted to be tachycardic. On further questioning, he also endorsed a 15-pound unintentional weight loss. Labs showed new anemia with Hgb of 6.1g/dL, leukocytosis with mild transaminitis, slightly elevated ALP, and LDH.
Abdominal imaging with CT revealed a 6 cm circumferential thickening of the hepatic flexure with multiple enhancing lesions in the liver, highly concerning for primary colonic neoplasm with possible metastatic disease. His CEA was noted to be in the 800ng/mL. An ultrasound-guided biopsy of the hepatic lesion showed moderate to poorly differentiated adenocarcinoma. Due to the metastatic disease, he was started on systemic chemotherapy with the FOLFOX regimen.
He presents again, now with worsening sepsis with Escherichia coli bacteremia and persistent penumobilia from his underlying cholecystocolonic fistula, complicated by multiple hepatic abscesses. He later underwent ultrasound-guided hepatic abscess drainage and external hepatic drain placement. Although his current presentation was managed symptomatically, he had progression of his malignancy despite chemotherapy that led to recurrent sepsis with worsening intestinal luminal obstruction that led to his untimely demise.
Discussion: Although rare, cholecystocolonic fistulas are almost always seen from underlying biliary tract disease as a primary mechanism of fistula formation. Our patient’s primary neoplastic colonic lesion eroding into the gallbladder led to the fistulous tract. Given the rapid disease progression and metastatic nature, options to treat the underlying CCF, in this case, were limited, leading to recurrent intraabdominal infections and sepsis. Although exceedingly rare, intestinal luminal malignancies should be on the differential for CCF and the subsequent pnuemobilia in the absence of an obvious primary gallbladder disease.

Disclosures:
Anuroop Yekula, MD1, Mythri Subramaniam, MD2, Anna Leszczynksi, MD2. P2990 - A Rare Presentation of Cholecystocolonic Fistula, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Vincent Hospital, Worcester, MA; 2Lahey Hospital, Burlington, MA
Introduction: Cholecystoenteric fistula is a rare disease that is usually seen with biliary pathologies. Cholecystocolonic fistulas (CCF) comprise at least 10-20% of cholecystoenteric fistulas. It is most commonly a result of biliary disease, especially cholelithiasis but also reported to be from abdominal trauma, IBD, and malignancy of the pancreaticobiliary system.
Here, we present a rare case of CCF from an occult luminal intestinal malignancy.
Case Description/Methods: A 45-year-old male with a medical history of type 1 diabetes initially presents with fatigue, nausea, and decreased appetite. His physical exam was unrevealing, but he was noted to be tachycardic. On further questioning, he also endorsed a 15-pound unintentional weight loss. Labs showed new anemia with Hgb of 6.1g/dL, leukocytosis with mild transaminitis, slightly elevated ALP, and LDH.
Abdominal imaging with CT revealed a 6 cm circumferential thickening of the hepatic flexure with multiple enhancing lesions in the liver, highly concerning for primary colonic neoplasm with possible metastatic disease. His CEA was noted to be in the 800ng/mL. An ultrasound-guided biopsy of the hepatic lesion showed moderate to poorly differentiated adenocarcinoma. Due to the metastatic disease, he was started on systemic chemotherapy with the FOLFOX regimen.
He presents again, now with worsening sepsis with Escherichia coli bacteremia and persistent penumobilia from his underlying cholecystocolonic fistula, complicated by multiple hepatic abscesses. He later underwent ultrasound-guided hepatic abscess drainage and external hepatic drain placement. Although his current presentation was managed symptomatically, he had progression of his malignancy despite chemotherapy that led to recurrent sepsis with worsening intestinal luminal obstruction that led to his untimely demise.
Discussion: Although rare, cholecystocolonic fistulas are almost always seen from underlying biliary tract disease as a primary mechanism of fistula formation. Our patient’s primary neoplastic colonic lesion eroding into the gallbladder led to the fistulous tract. Given the rapid disease progression and metastatic nature, options to treat the underlying CCF, in this case, were limited, leading to recurrent intraabdominal infections and sepsis. Although exceedingly rare, intestinal luminal malignancies should be on the differential for CCF and the subsequent pnuemobilia in the absence of an obvious primary gallbladder disease.

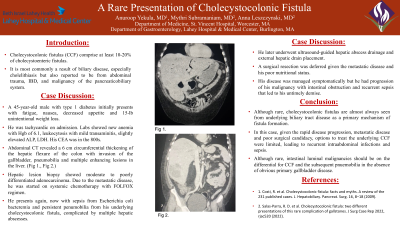
Figure:
Fig 1.: Pneumobilia with air in the biliary tree and the gallbladder.
Fig 2.: Choledochocolonic fistula with the apparent connection of gallbladder and the ascending colon.
Fig 1.: Pneumobilia with air in the biliary tree and the gallbladder.
Fig 2.: Choledochocolonic fistula with the apparent connection of gallbladder and the ascending colon.
Disclosures:
Anuroop Yekula indicated no relevant financial relationships.
Mythri Subramaniam indicated no relevant financial relationships.
Anna Leszczynksi indicated no relevant financial relationships.
Anuroop Yekula, MD1, Mythri Subramaniam, MD2, Anna Leszczynksi, MD2. P2990 - A Rare Presentation of Cholecystocolonic Fistula, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

