Tuesday Poster Session
Category: Biliary/Pancreas
P2992 - Bile Cast Syndrome in a Young Female Following Severe COVID-19 Infection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MF
Maryam Farooq, MSEd
David Geffen School of Medicine at University of California Los Angeles
Los Angeles, CA
Presenting Author(s)
Award: Presidential Poster Award
Maryam Farooq, MSEd1, Sentia Irania, MD2, Firas Bahdi, MD3, Beshoy Yanny, MD3, Danny Issa, MD3
1David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA; 2Ronald Reagan Hospital, Los Angeles, CA; 3UCLA, Los Angeles, CA
Introduction: Post-COVID-19 cholangiopathy is a rare entity that remains poorly understood. Bile cast syndrome is an unusual complication typically reported in patients following liver transplant. Here we describe a unique case of bile cast syndrome developed as a late complication of severe COVID-19 in a young, otherwise healthy female and further discuss therapeutic techniques.
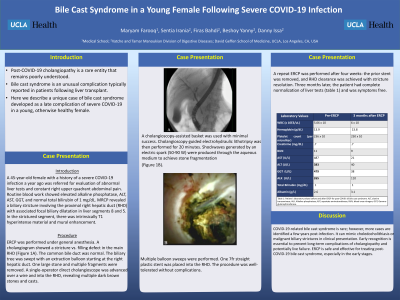
Case Description/Methods: A 45-year-old female with a history of a severe COVID-19 infection a year ago was referred for evaluation of abnormal liver tests and constant right upper quadrant abdominal pain. Routine blood work showed elevated alkaline phosphatase at 265 U/L, ALT 107 U/L, AST 62 U/L, GGT 479 U/L, and normal total bilirubin of 1 mg/dL. MR cholangiopancreatogram revealed a biliary stricture involving the proximal right hepatic duct (RHD) with associated focal biliary dilatation in liver segments 8 and 5. In the strictured segment, there was intrinsically T1 hyperintense material and mural enhancement. ERCP was performed under general anesthesia. A cholangiogram showed a stricture vs. filling defect in the main RHD (Figure 1A). The common bile duct was normal. The biliary tree was swept with an extraction balloon starting at the right hepatic duct. One large stone and multiple fragments were removed. A single-operator direct cholangioscope was advanced over a wire and into the RHD, revealing multiple dark brown stones and casts. A cholangioscopy-assisted basket was used with minimal success. Cholangioscopy-guided electrohydraulic lithotripsy was then performed for 20 minutes. Shockwaves generated by an electric spark (50-90 W) were produced through the aqueous medium to achieve stone fragmentation (Figure 1B, C). Multiple balloon sweeps were performed. One 7fr straight plastic stent was placed into the RHD. The procedure was well-tolerated without complications. A repeat ERCP was performed after four weeks: the prior stent was removed, and RHD clearance was achieved with stricture resolution. Three months later, the patient had complete normalization of liver tests (table 1) and was symptoms free.
Discussion: COVID-19-related bile cast syndrome is rare; however, more cases are identified a few years post-infection. It can mimic choledocholithiasis or malignant biliary strictures in clinical presentation. Early recognition is essential to prevent long-term complications of cholangiopathy and potentially live failure. ERCP is safe and effective for treating post-COVID-19 bile cast syndrome, especially in the early stages.

Disclosures:
Maryam Farooq, MSEd1, Sentia Irania, MD2, Firas Bahdi, MD3, Beshoy Yanny, MD3, Danny Issa, MD3. P2992 - Bile Cast Syndrome in a Young Female Following Severe COVID-19 Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Maryam Farooq, MSEd1, Sentia Irania, MD2, Firas Bahdi, MD3, Beshoy Yanny, MD3, Danny Issa, MD3
1David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA; 2Ronald Reagan Hospital, Los Angeles, CA; 3UCLA, Los Angeles, CA
Introduction: Post-COVID-19 cholangiopathy is a rare entity that remains poorly understood. Bile cast syndrome is an unusual complication typically reported in patients following liver transplant. Here we describe a unique case of bile cast syndrome developed as a late complication of severe COVID-19 in a young, otherwise healthy female and further discuss therapeutic techniques.
Case Description/Methods: A 45-year-old female with a history of a severe COVID-19 infection a year ago was referred for evaluation of abnormal liver tests and constant right upper quadrant abdominal pain. Routine blood work showed elevated alkaline phosphatase at 265 U/L, ALT 107 U/L, AST 62 U/L, GGT 479 U/L, and normal total bilirubin of 1 mg/dL. MR cholangiopancreatogram revealed a biliary stricture involving the proximal right hepatic duct (RHD) with associated focal biliary dilatation in liver segments 8 and 5. In the strictured segment, there was intrinsically T1 hyperintense material and mural enhancement. ERCP was performed under general anesthesia. A cholangiogram showed a stricture vs. filling defect in the main RHD (Figure 1A). The common bile duct was normal. The biliary tree was swept with an extraction balloon starting at the right hepatic duct. One large stone and multiple fragments were removed. A single-operator direct cholangioscope was advanced over a wire and into the RHD, revealing multiple dark brown stones and casts. A cholangioscopy-assisted basket was used with minimal success. Cholangioscopy-guided electrohydraulic lithotripsy was then performed for 20 minutes. Shockwaves generated by an electric spark (50-90 W) were produced through the aqueous medium to achieve stone fragmentation (Figure 1B, C). Multiple balloon sweeps were performed. One 7fr straight plastic stent was placed into the RHD. The procedure was well-tolerated without complications. A repeat ERCP was performed after four weeks: the prior stent was removed, and RHD clearance was achieved with stricture resolution. Three months later, the patient had complete normalization of liver tests (table 1) and was symptoms free.
Discussion: COVID-19-related bile cast syndrome is rare; however, more cases are identified a few years post-infection. It can mimic choledocholithiasis or malignant biliary strictures in clinical presentation. Early recognition is essential to prevent long-term complications of cholangiopathy and potentially live failure. ERCP is safe and effective for treating post-COVID-19 bile cast syndrome, especially in the early stages.

Figure: Figure 1A: Fluroscopy image of cholangioscopy guided cannulation of the right hepatic duct
Figure1B: Cholangioscopy view of bile casts inside the right hepatic duct
Figure 1C: Cholangioscopy guided lithortripsy of the bile casts
Figure1B: Cholangioscopy view of bile casts inside the right hepatic duct
Figure 1C: Cholangioscopy guided lithortripsy of the bile casts
Disclosures:
Maryam Farooq indicated no relevant financial relationships.
Sentia Irania indicated no relevant financial relationships.
Firas Bahdi indicated no relevant financial relationships.
Beshoy Yanny indicated no relevant financial relationships.
Danny Issa indicated no relevant financial relationships.
Maryam Farooq, MSEd1, Sentia Irania, MD2, Firas Bahdi, MD3, Beshoy Yanny, MD3, Danny Issa, MD3. P2992 - Bile Cast Syndrome in a Young Female Following Severe COVID-19 Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

