Tuesday Poster Session
Category: Biliary/Pancreas
P2993 - Intervening on a Complex Case of Pancreatic Injury in a High-Risk Patient
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ashley Long, DO
HCA Florida Largo Hospital
Largo, FL
Presenting Author(s)
Ashley Long, DO1, Blake Flores Semyonov, DO1, Jay Patel, MD2, Anabel Rodriguez Loya, DO1, Yevgeniya Goltser, DO1, Bobby Jacob, MD1, Meir Mizrahi, MD1, Patricia Chun, DO1
1HCA Florida Largo Hospital, Largo, FL; 2HCA Florida Orange Park Hospital, Orange Park, FL
Introduction: Pancreatic injury is a rare complication of abdominal trauma, with significant morbidity and mortality rates. It can be difficult to diagnose traumatic pancreatic injury because its presentation may be non-specific. MRCP is an effective, non-invasive diagnostic tool used to detect pancreatic duct (PD) injury.
Necrotizing pancreatitis is a complication in 10% and pancreatic pseudocyst up to 18% of all cases of acute pancreatitis, with a mortality of 17%. Previously, open necrosectomy was the mainstay of treatment but less invasive techniques have overtaken it due to its high morbidity.
Case Description/Methods: A 31-year-old female with a history of pancreatitis and 3 days of constant, stabbing epigastric abdominal pain following a scooter accident presented for advanced endoscopy evaluation. Labs were significant for WBC 14.3, lactic acid 2.7, and lipase 1370.
CT showed worsening of a multiloculated uncinate pseudocyst, progression of necrosis, and multifocal pancreatic duct transection (Figure 1). MRI Abdomen confirmed the findings of multifocal pancreatic duct injury involving the midbody of the pancreas (Grade III) and an associated large complex multiloculated acute peripancreatic fluid collection.
Four days later, CT Abdomen/Pelvis showed maturation of severe necrotizing pancreatitis and multi-spatial fluid collection/phlegmon. Subsequent ERCP and EUS were performed and a plastic PD stent and lumen apposing metal stent (LAMS) was placed within the pseudocyst.
Four days later, CT Abdomen/Pelvis showed decreased pseudocyst size with subsequent EGD with necrosectomy being performed. The following week, LAMS was removed. The patient’s pain resolved and she was recommended to repeat EGD/ERCP in 6-8 weeks.
Discussion: This case emphasizes the importance of early diagnosis and intervention of pancreatic injury for optimal patient outcomes. While advanced endoscopy is not readily accessible, it is imperative that diagnosis is made early and GI feedback is obtained for possible transfer to an advanced endoscopist or for surgical intervention.
Our patient with a grade III injury and pseudocyst was successfully treated endoscopically, sparing her from an invasive surgical procedure with increased complication risks. Endoscopic drainage has been shown to have an efficacy to that of surgery, attesting to the advancements in the field providing alternative treatments.

Disclosures:
Ashley Long, DO1, Blake Flores Semyonov, DO1, Jay Patel, MD2, Anabel Rodriguez Loya, DO1, Yevgeniya Goltser, DO1, Bobby Jacob, MD1, Meir Mizrahi, MD1, Patricia Chun, DO1. P2993 - Intervening on a Complex Case of Pancreatic Injury in a High-Risk Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1HCA Florida Largo Hospital, Largo, FL; 2HCA Florida Orange Park Hospital, Orange Park, FL
Introduction: Pancreatic injury is a rare complication of abdominal trauma, with significant morbidity and mortality rates. It can be difficult to diagnose traumatic pancreatic injury because its presentation may be non-specific. MRCP is an effective, non-invasive diagnostic tool used to detect pancreatic duct (PD) injury.
Necrotizing pancreatitis is a complication in 10% and pancreatic pseudocyst up to 18% of all cases of acute pancreatitis, with a mortality of 17%. Previously, open necrosectomy was the mainstay of treatment but less invasive techniques have overtaken it due to its high morbidity.
Case Description/Methods: A 31-year-old female with a history of pancreatitis and 3 days of constant, stabbing epigastric abdominal pain following a scooter accident presented for advanced endoscopy evaluation. Labs were significant for WBC 14.3, lactic acid 2.7, and lipase 1370.
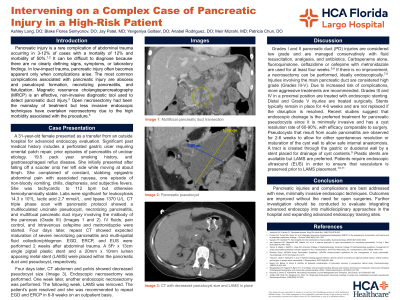
CT showed worsening of a multiloculated uncinate pseudocyst, progression of necrosis, and multifocal pancreatic duct transection (Figure 1). MRI Abdomen confirmed the findings of multifocal pancreatic duct injury involving the midbody of the pancreas (Grade III) and an associated large complex multiloculated acute peripancreatic fluid collection.
Four days later, CT Abdomen/Pelvis showed maturation of severe necrotizing pancreatitis and multi-spatial fluid collection/phlegmon. Subsequent ERCP and EUS were performed and a plastic PD stent and lumen apposing metal stent (LAMS) was placed within the pseudocyst.
Four days later, CT Abdomen/Pelvis showed decreased pseudocyst size with subsequent EGD with necrosectomy being performed. The following week, LAMS was removed. The patient’s pain resolved and she was recommended to repeat EGD/ERCP in 6-8 weeks.
Discussion: This case emphasizes the importance of early diagnosis and intervention of pancreatic injury for optimal patient outcomes. While advanced endoscopy is not readily accessible, it is imperative that diagnosis is made early and GI feedback is obtained for possible transfer to an advanced endoscopist or for surgical intervention.
Our patient with a grade III injury and pseudocyst was successfully treated endoscopically, sparing her from an invasive surgical procedure with increased complication risks. Endoscopic drainage has been shown to have an efficacy to that of surgery, attesting to the advancements in the field providing alternative treatments.

Figure: Figure 1: Multifocal Pancreatic Duct Transection
Disclosures:
Ashley Long indicated no relevant financial relationships.
Blake Flores Semyonov indicated no relevant financial relationships.
Jay Patel indicated no relevant financial relationships.
Anabel Rodriguez Loya indicated no relevant financial relationships.
Yevgeniya Goltser indicated no relevant financial relationships.
Bobby Jacob indicated no relevant financial relationships.
Meir Mizrahi indicated no relevant financial relationships.
Patricia Chun indicated no relevant financial relationships.
Ashley Long, DO1, Blake Flores Semyonov, DO1, Jay Patel, MD2, Anabel Rodriguez Loya, DO1, Yevgeniya Goltser, DO1, Bobby Jacob, MD1, Meir Mizrahi, MD1, Patricia Chun, DO1. P2993 - Intervening on a Complex Case of Pancreatic Injury in a High-Risk Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
