Tuesday Poster Session
Category: Biliary/Pancreas
P2997 - A Rare Association of Protease Inhibitors With Acute Pancreatitis: A Case Report
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Khalid Ahmed, MD
The Wright Center for GME
Scranton, PA
Presenting Author(s)
Khalid Ahmed, MD1, Peter Iskander, MD2, Syed Muhammad Hussain Zaidi, MD3, Elmkdad Mohammed, MD1, Ayman Elawad, MD4, Beshir Saeed, MD5
1The Wright Center for GME, Scranton, PA; 2The Wright Center for GME, Dunmore, PA; 3Wright Center, Scranton, PA; 4Howard University Hospital, Washington, DC; 5Jefferson Lansdale Hospital, Lansdale, PA
Introduction: The most common cause of acute pancreatitis (AP) is gallstones, followed by alcohol use in the US. Drug-induced pancreatitis accounts for only < 5% of the cases. According to WHO, more than 500 medications have been identified to possibly induce pancreatitis, with less than 50 medications determined to have a plausible causality. We present a case of an association between the use of protease inhibitor (PI) Nirmatrelvir / Ritonavir prescribed to a patient diagnosed with COVID-19 infection; and the subsequent development of AP.
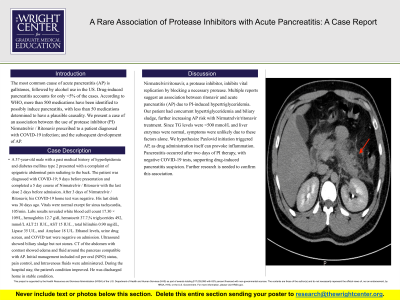
Case Description/Methods: A 37-year-old male with a past medical history of hyperlipidemia and diabetes mellitus type 2 presented with a complaint of epigastric abdominal pain radiating to the back. The patient was diagnosed with COVID-19; 9 days before presentation and completed a 5 day course of Nirmatrelvir / Ritonavir with the last dose 2 days before admission. After 3 days of Nirmatrelvir / Ritonavir, his COVID-19 home test was negative. His last drink was 30 days ago. Vitals were normal except for sinus tachycardia, 105/min. Labs results revealed white blood cell count 17.30 × 109/L, hemoglobin 12.7 g/dl, hematocrit 37.7,% triglycerides 492, mmol/L ALT 21 IU/L, AST 15 IU/L , total bilirubin 0.90 mg/dL, Lipase 35 U/L, and Amylase 18 U/L. Ethanol levels, urine drug screen, and COVID test were negative on admission. Ultrasound showed biliary sludge but not stones. CT of the abdomen with contrast showed edema and fluid around the pancreas compatible with AP. Initial management included nil per oral (NPO) status, pain control, and Intravenous fluids were administered. During the hospital stay, the patient's condition improved. He was discharged home in stable condition.
Discussion: Nirmatrelvir/ritonavir, a protease inhibitor, inhibits vital replication by blocking a necessary protease. Multiple reports suggest an association between ritonavir and acute pancreatitis (AP) due to PI-induced hypertriglyceridemia. Our patient had concurrent hypertriglyceridemia and biliary sludge, further increasing AP risk with Nirmatrelvir/ritonavir treatment. Since TG levels were < 500 mmol/L and liver enzymes were normal, symptoms were unlikely due to these factors alone. We hypothesize Paxlovid initiation triggered AP, as drug administration itself can provoke inflammation. Pancreatitis occurred after two days of PI therapy, with negative COVID-19 tests, supporting drug-induced pancreatitis suspicion. Further research is needed to confirm this association.

Disclosures:
Khalid Ahmed, MD1, Peter Iskander, MD2, Syed Muhammad Hussain Zaidi, MD3, Elmkdad Mohammed, MD1, Ayman Elawad, MD4, Beshir Saeed, MD5. P2997 - A Rare Association of Protease Inhibitors With Acute Pancreatitis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1The Wright Center for GME, Scranton, PA; 2The Wright Center for GME, Dunmore, PA; 3Wright Center, Scranton, PA; 4Howard University Hospital, Washington, DC; 5Jefferson Lansdale Hospital, Lansdale, PA
Introduction: The most common cause of acute pancreatitis (AP) is gallstones, followed by alcohol use in the US. Drug-induced pancreatitis accounts for only < 5% of the cases. According to WHO, more than 500 medications have been identified to possibly induce pancreatitis, with less than 50 medications determined to have a plausible causality. We present a case of an association between the use of protease inhibitor (PI) Nirmatrelvir / Ritonavir prescribed to a patient diagnosed with COVID-19 infection; and the subsequent development of AP.
Case Description/Methods: A 37-year-old male with a past medical history of hyperlipidemia and diabetes mellitus type 2 presented with a complaint of epigastric abdominal pain radiating to the back. The patient was diagnosed with COVID-19; 9 days before presentation and completed a 5 day course of Nirmatrelvir / Ritonavir with the last dose 2 days before admission. After 3 days of Nirmatrelvir / Ritonavir, his COVID-19 home test was negative. His last drink was 30 days ago. Vitals were normal except for sinus tachycardia, 105/min. Labs results revealed white blood cell count 17.30 × 109/L, hemoglobin 12.7 g/dl, hematocrit 37.7,% triglycerides 492, mmol/L ALT 21 IU/L, AST 15 IU/L , total bilirubin 0.90 mg/dL, Lipase 35 U/L, and Amylase 18 U/L. Ethanol levels, urine drug screen, and COVID test were negative on admission. Ultrasound showed biliary sludge but not stones. CT of the abdomen with contrast showed edema and fluid around the pancreas compatible with AP. Initial management included nil per oral (NPO) status, pain control, and Intravenous fluids were administered. During the hospital stay, the patient's condition improved. He was discharged home in stable condition.
Discussion: Nirmatrelvir/ritonavir, a protease inhibitor, inhibits vital replication by blocking a necessary protease. Multiple reports suggest an association between ritonavir and acute pancreatitis (AP) due to PI-induced hypertriglyceridemia. Our patient had concurrent hypertriglyceridemia and biliary sludge, further increasing AP risk with Nirmatrelvir/ritonavir treatment. Since TG levels were < 500 mmol/L and liver enzymes were normal, symptoms were unlikely due to these factors alone. We hypothesize Paxlovid initiation triggered AP, as drug administration itself can provoke inflammation. Pancreatitis occurred after two days of PI therapy, with negative COVID-19 tests, supporting drug-induced pancreatitis suspicion. Further research is needed to confirm this association.

Figure: Figure 1. CT scan showing evidence of Acute Pancreatitis.
Disclosures:
Khalid Ahmed indicated no relevant financial relationships.
Peter Iskander indicated no relevant financial relationships.
Syed Muhammad Hussain Zaidi indicated no relevant financial relationships.
Elmkdad Mohammed indicated no relevant financial relationships.
Ayman Elawad indicated no relevant financial relationships.
Beshir Saeed indicated no relevant financial relationships.
Khalid Ahmed, MD1, Peter Iskander, MD2, Syed Muhammad Hussain Zaidi, MD3, Elmkdad Mohammed, MD1, Ayman Elawad, MD4, Beshir Saeed, MD5. P2997 - A Rare Association of Protease Inhibitors With Acute Pancreatitis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
