Tuesday Poster Session
Category: Colon
P3000 - COVID-19 and Venous Thromboembolism Among Patients With Gastrointestinal Malignancies: A Nationwide Inpatient Sample Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Muhammad Bilal Ibrahim, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Hiba Noor, MBBS1, Muhammad Bilal Ibrahim, MD2, Ali Husnain, MBBS3, Ayobami Olafimihan, MD2, Mihir Prakash Shah, MD2, Chun-Wei Pan, MD2, Rafaella Litvin, MD2
1Fatima Jinnah Medical University, Lahore, Punjab, Pakistan; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Sahara Medical College, Narowal, Punjab, Pakistan
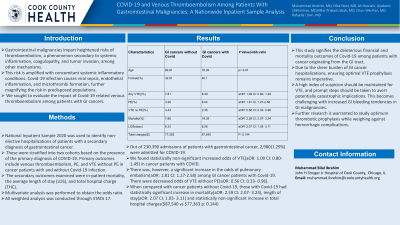
Introduction: Gastrointestinal malignancies impart heightened risks of thromboembolism, a phenomenon secondary to systemic inflammation, coagulopathy, and tumor invasion, among other mechanisms. This risk is amplified with concomitant systemic inflammatory conditions. Covid-19 infection causes viral sepsis, endothelial inflammation, and microthrombi formation, further magnifying the risk in predisposed populations. We sought to evaluate the impact of Covid-19 related venous thromboembolism among patients with GI cancers.
Methods: National Inpatient Sample 2020 was used to identify non-elective hospitalizations of patients with a secondary diagnosis of gastrointestinal cancer. These were stratified into two cohorts based on the presence of the primary diagnosis of COVID-19. Primary outcomes include venous thromboembolism, PE, and VTE without PE in cancer patients with and without Covid-19 infection. The secondary outcomes examined were in-patient mortality, the average length of stay (LOS), and total hospital charge (THC). Multivariate analysis was performed to obtain the odds ratio. All weighted analysis was conducted through STATA 17.
Results: Out of 230,390 admissions of patients with gastrointestinal cancer, 2,980(1.29%) were admitted for COVID-19. We found statistically non-significant increased odds of VTE(aOR: 1.09 CI: 0.80- 1.49) in cancer patients with COVID. There was, however, a significant increase in the odds of pulmonary embolism(aOR: 1.81 CI: 1.27-2.58) among GI cancer patients with Covid-19. There were decreased odds of VTE without PE(aOR: 0.56 CI: 0.33- 0.96). When compared with cancer patients without Covid-19, those with Covid-19 had statistically significant increase in mortality(aOR: 2.59 CI: 2.07- 3.24), length of stay(aOR: 2.07 CI: 1.03- 3.11) and statistically non-significant increase in total hospital charges($87,540 vs $77,363 p: 0.144)
Discussion: This study signifies the deleterious financial and mortality outcomes of Covid-19 among patients with cancer originating from the GI tract. Due to the sheer burden of GI cancer hospitalizations, ensuring optimal VTE prophylaxis remains imperative. A high index of suspicion should be maintained for VTE, and prompt steps should be taken to avert potentially catastrophic implications. This becomes challenging with increased GI bleeding tendencies in GI malignancies. Further research is warranted to study optimum thrombotic prophylaxis while weighing against hemorrhagic complications.
Disclosures:
Hiba Noor, MBBS1, Muhammad Bilal Ibrahim, MD2, Ali Husnain, MBBS3, Ayobami Olafimihan, MD2, Mihir Prakash Shah, MD2, Chun-Wei Pan, MD2, Rafaella Litvin, MD2. P3000 - COVID-19 and Venous Thromboembolism Among Patients With Gastrointestinal Malignancies: A Nationwide Inpatient Sample Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Fatima Jinnah Medical University, Lahore, Punjab, Pakistan; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Sahara Medical College, Narowal, Punjab, Pakistan
Introduction: Gastrointestinal malignancies impart heightened risks of thromboembolism, a phenomenon secondary to systemic inflammation, coagulopathy, and tumor invasion, among other mechanisms. This risk is amplified with concomitant systemic inflammatory conditions. Covid-19 infection causes viral sepsis, endothelial inflammation, and microthrombi formation, further magnifying the risk in predisposed populations. We sought to evaluate the impact of Covid-19 related venous thromboembolism among patients with GI cancers.
Methods: National Inpatient Sample 2020 was used to identify non-elective hospitalizations of patients with a secondary diagnosis of gastrointestinal cancer. These were stratified into two cohorts based on the presence of the primary diagnosis of COVID-19. Primary outcomes include venous thromboembolism, PE, and VTE without PE in cancer patients with and without Covid-19 infection. The secondary outcomes examined were in-patient mortality, the average length of stay (LOS), and total hospital charge (THC). Multivariate analysis was performed to obtain the odds ratio. All weighted analysis was conducted through STATA 17.
Results: Out of 230,390 admissions of patients with gastrointestinal cancer, 2,980(1.29%) were admitted for COVID-19. We found statistically non-significant increased odds of VTE(aOR: 1.09 CI: 0.80- 1.49) in cancer patients with COVID. There was, however, a significant increase in the odds of pulmonary embolism(aOR: 1.81 CI: 1.27-2.58) among GI cancer patients with Covid-19. There were decreased odds of VTE without PE(aOR: 0.56 CI: 0.33- 0.96). When compared with cancer patients without Covid-19, those with Covid-19 had statistically significant increase in mortality(aOR: 2.59 CI: 2.07- 3.24), length of stay(aOR: 2.07 CI: 1.03- 3.11) and statistically non-significant increase in total hospital charges($87,540 vs $77,363 p: 0.144)
Discussion: This study signifies the deleterious financial and mortality outcomes of Covid-19 among patients with cancer originating from the GI tract. Due to the sheer burden of GI cancer hospitalizations, ensuring optimal VTE prophylaxis remains imperative. A high index of suspicion should be maintained for VTE, and prompt steps should be taken to avert potentially catastrophic implications. This becomes challenging with increased GI bleeding tendencies in GI malignancies. Further research is warranted to study optimum thrombotic prophylaxis while weighing against hemorrhagic complications.
Disclosures:
Hiba Noor indicated no relevant financial relationships.
Muhammad Bilal Ibrahim indicated no relevant financial relationships.
Ali Husnain indicated no relevant financial relationships.
Ayobami Olafimihan indicated no relevant financial relationships.
Mihir Prakash Shah indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Rafaella Litvin indicated no relevant financial relationships.
Hiba Noor, MBBS1, Muhammad Bilal Ibrahim, MD2, Ali Husnain, MBBS3, Ayobami Olafimihan, MD2, Mihir Prakash Shah, MD2, Chun-Wei Pan, MD2, Rafaella Litvin, MD2. P3000 - COVID-19 and Venous Thromboembolism Among Patients With Gastrointestinal Malignancies: A Nationwide Inpatient Sample Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
