Tuesday Poster Session
Category: Liver
P4002 - A Protein Paradox: A Case of Spontaneous Portosystemic Shunt Encephalopathy and Protein-Losing Enteropathy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Mariko Maxwell, MD
Yale University School of Medicine
Middlefield, CT
Presenting Author(s)
Mariko Maxwell, MD1, Catherine Mezzacappa, MD, MPH2, Nadeen Hussain, MD2, Petr Protiva, MD, MPH3, Joshua Cornman-Homonoff, MD4, Paul DiDomenico, MD5, Gyanprakash Ketwaroo, MD2, Tamar Taddei, MD3
1Yale University School of Medicine, Middlefield, CT; 2Yale University School of Medicine, New Haven, CT; 3Yale University School of Medicine and VA Connecticut Healthcare System, New Haven, CT; 4Yale University School of Medicine, Old Saybrook, CT; 5Yale University School of Medicine, West Haven, CT
Introduction: The recognition of type B hepatic encephalopathy – portosystemic shunting without hepatic dysfunction – is challenging given its rarity. While many cases are spontaneous, high protein intake has been identified as a precipitant. Another rare condition – protein-losing enteropathy – characterized by excessive protein loss due to variable underlying gastrointestinal pathologies, is treated with protein supplementation. We describe a challenging diagnostic case of co-occurring protein-losing enteropathy and non-cirrhotic portosystemic encephalopathy.
Case Description/Methods: A 56-year-old male with past medical history of diverticulitis status post partial colectomy, prior duodenal perforation and ischemic colitis, and coronary artery disease presented with two weeks of frequent falls and diffuse edema. Notably, he was admitted three times in the preceding months with abdominal pain, found to have over 30 gastroduodenal ulcers on endoscopy, and diffuse bowel wall thickening with ileitis on abdominal computed tomography (CT).
Initial physical exam was notable for asterixis, anasarca, and agitation alternating with somnolence. Laboratory studies revealed a serum albumin of 1.1 g/dL, normal immunoglobulin levels, trace urine protein, serum alkaline phosphatase of 292 IU/L, normal total bilirubin, normal AST and ALT, and ammonia of 110 µg/dL. The patient was initiated on lactulose with resolution of encephalopathy. His albumin remained ≤ 1.1 g/dL but protein supplementation was avoided in the setting of encephalopathy of unknown etiology. Abdominal CT revealed a spontaneous splenorenal shunt (Figure 1). The patient underwent transjugular renal venogram followed by splenorenal shunt coil and vascular plug embolization. At one-week follow up, he was without evidence of encephalopathy. Bi-directional endoscopy was recommended but patient declined colonoscopy. Upper endoscopy revealed gastric scarring. At the time of writing, he is pending drainage of a peri-gastric fluid collection.
Discussion: The diagnosis of non-cirrhotic portosystemic encephalopathy can be challenging due to its rarity. In this case report, we discuss the workup that led to the diagnosis of type B encephalopathy in a patient with likely co-occurring protein-losing enteropathy. The presence of both rare disorders presented not only a diagnostic challenge, but therapeutic as well, as the treatment for the latter disorder can serve as a trigger of the former.

Disclosures:
Mariko Maxwell, MD1, Catherine Mezzacappa, MD, MPH2, Nadeen Hussain, MD2, Petr Protiva, MD, MPH3, Joshua Cornman-Homonoff, MD4, Paul DiDomenico, MD5, Gyanprakash Ketwaroo, MD2, Tamar Taddei, MD3. P4002 - A Protein Paradox: A Case of Spontaneous Portosystemic Shunt Encephalopathy and Protein-Losing Enteropathy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale University School of Medicine, Middlefield, CT; 2Yale University School of Medicine, New Haven, CT; 3Yale University School of Medicine and VA Connecticut Healthcare System, New Haven, CT; 4Yale University School of Medicine, Old Saybrook, CT; 5Yale University School of Medicine, West Haven, CT
Introduction: The recognition of type B hepatic encephalopathy – portosystemic shunting without hepatic dysfunction – is challenging given its rarity. While many cases are spontaneous, high protein intake has been identified as a precipitant. Another rare condition – protein-losing enteropathy – characterized by excessive protein loss due to variable underlying gastrointestinal pathologies, is treated with protein supplementation. We describe a challenging diagnostic case of co-occurring protein-losing enteropathy and non-cirrhotic portosystemic encephalopathy.
Case Description/Methods: A 56-year-old male with past medical history of diverticulitis status post partial colectomy, prior duodenal perforation and ischemic colitis, and coronary artery disease presented with two weeks of frequent falls and diffuse edema. Notably, he was admitted three times in the preceding months with abdominal pain, found to have over 30 gastroduodenal ulcers on endoscopy, and diffuse bowel wall thickening with ileitis on abdominal computed tomography (CT).
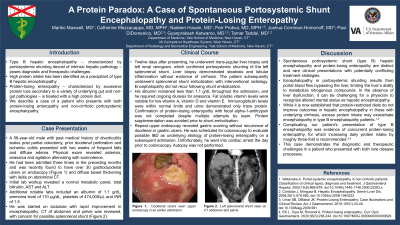
Initial physical exam was notable for asterixis, anasarca, and agitation alternating with somnolence. Laboratory studies revealed a serum albumin of 1.1 g/dL, normal immunoglobulin levels, trace urine protein, serum alkaline phosphatase of 292 IU/L, normal total bilirubin, normal AST and ALT, and ammonia of 110 µg/dL. The patient was initiated on lactulose with resolution of encephalopathy. His albumin remained ≤ 1.1 g/dL but protein supplementation was avoided in the setting of encephalopathy of unknown etiology. Abdominal CT revealed a spontaneous splenorenal shunt (Figure 1). The patient underwent transjugular renal venogram followed by splenorenal shunt coil and vascular plug embolization. At one-week follow up, he was without evidence of encephalopathy. Bi-directional endoscopy was recommended but patient declined colonoscopy. Upper endoscopy revealed gastric scarring. At the time of writing, he is pending drainage of a peri-gastric fluid collection.
Discussion: The diagnosis of non-cirrhotic portosystemic encephalopathy can be challenging due to its rarity. In this case report, we discuss the workup that led to the diagnosis of type B encephalopathy in a patient with likely co-occurring protein-losing enteropathy. The presence of both rare disorders presented not only a diagnostic challenge, but therapeutic as well, as the treatment for the latter disorder can serve as a trigger of the former.

Figure: Figure 1. Left splenorenal shunt seen on CT scan of the abdomen and pelvis.
Disclosures:
Mariko Maxwell indicated no relevant financial relationships.
Catherine Mezzacappa indicated no relevant financial relationships.
Nadeen Hussain indicated no relevant financial relationships.
Petr Protiva indicated no relevant financial relationships.
Joshua Cornman-Homonoff: Inari Medical – Single lecture 1.5 years ago.
Paul DiDomenico indicated no relevant financial relationships.
Gyanprakash Ketwaroo indicated no relevant financial relationships.
Tamar Taddei: American Association for the Study of Liver Diseases – Advisory Committee/Board Member.
Mariko Maxwell, MD1, Catherine Mezzacappa, MD, MPH2, Nadeen Hussain, MD2, Petr Protiva, MD, MPH3, Joshua Cornman-Homonoff, MD4, Paul DiDomenico, MD5, Gyanprakash Ketwaroo, MD2, Tamar Taddei, MD3. P4002 - A Protein Paradox: A Case of Spontaneous Portosystemic Shunt Encephalopathy and Protein-Losing Enteropathy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
