Tuesday Poster Session
Category: Liver
P4014 - Hepatic Abscess Development Following Locoregional Therapy for Hepatocellular Carcinoma in Patients With Decompensated Cirrhosis & Prior Biliary Manipulation: A Case Series
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Vinay Rao, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Vinay Rao, MD, Salil Chowdhury, MD, Jonathan Gross, MD, JD, Justin Bilello, MD, Beatriz Torre, MD, Dina Halegoua-DeMarzio, MD
Thomas Jefferson University Hospital, Philadelphia, PA
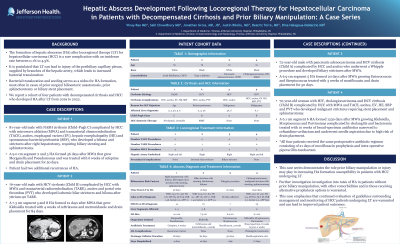
Introduction: The formation of hepatic abscesses (HA) after locoregional therapy (LT) for hepatocellular carcinoma (HCC) is a rare complication. It is postulated that prior bacterial seeding of peribiliary capillaries acts as a nidus for HA. We report a cohort of four patients with decompensated cirrhosis and HCC who developed HA after LT from 2019 to 2022.
Case Description/Methods: Patient 1 is an 81-year-old male with NASH cirrhosis (Child-Pugh C) complicated by HCC with microwave ablation (MWA) and transarterial chemoembolization (TACE), ascites, esophageal varices (EV), hepatic encephalopathy (HE) and spontaneous bacterial peritonitis (SBP), who developed biloma and strictures after right hepatectomy, requiring stenting and sphincterotomy. A 9.0 cm segment 2 and 3 HA formed 56 days after MWA growing Morganella and Pseudomonas treated with 6 weeks cefepime and drain placement for 50 days. He had two more recurrences of HA.
Patient 2 is a 76-year-old male with HCV cirrhosis (Child B) complicated by HCC with MWA and transarterial radioembolization (TARE), ascites and portal vein thrombus (PVT) who developed ischemic hilar strictures and biloma after yttrium-90 TARE. A 7.3 cm segment 5 and 8 HA formed 12 days after MWA growing Klebsiella treated with 4 weeks ceftriaxone and metronidazole and drain placement for 84 days.
Patient 3 is a 72-year-old male with pancreatic adenocarcinoma and HCV cirrhosis (Child A) complicated by HCC and ascites who underwent Whipple procedure and developed biliary strictures after MWA. A 6.9 cm segment 5 HA formed 20 days after MWA growing Enterococcus and Streptococcus treated with 3 weeks moxifloxacin and drain placement for 50 days.
Patient 4 is a 70-year-old woman with HIV, cholangiocarcinoma and HCV cirrhosis (Child B) complicated by HCC with MWA and TACE, ascites, EV, HE, SBP and PVT who developed malignant strictures requiring stents and sphincterotomy. A 6.1 cm segment 6 HA formed 1230 days after MWA growing Klebsiella, Streptococcus and Parvinomas complicated by cholangitis and bacteremia treated with 10 weeks of antibiotics narrowed to ceftazidime-avibactam and needle aspiration.
All patients received the same perioperative antibiotic prophylaxis.
Discussion: This case series demonstrates the role prior biliary manipulation may play in increasing susceptibility to HA formation in HCC patients undergoing LT. Further investigation into rates of HA in patients without biliary manipulation, with other comorbidities, and those receiving alternative prophylaxis is warranted.
Disclosures:
Vinay Rao, MD, Salil Chowdhury, MD, Jonathan Gross, MD, JD, Justin Bilello, MD, Beatriz Torre, MD, Dina Halegoua-DeMarzio, MD. P4014 - Hepatic Abscess Development Following Locoregional Therapy for Hepatocellular Carcinoma in Patients With Decompensated Cirrhosis & Prior Biliary Manipulation: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: The formation of hepatic abscesses (HA) after locoregional therapy (LT) for hepatocellular carcinoma (HCC) is a rare complication. It is postulated that prior bacterial seeding of peribiliary capillaries acts as a nidus for HA. We report a cohort of four patients with decompensated cirrhosis and HCC who developed HA after LT from 2019 to 2022.
Case Description/Methods: Patient 1 is an 81-year-old male with NASH cirrhosis (Child-Pugh C) complicated by HCC with microwave ablation (MWA) and transarterial chemoembolization (TACE), ascites, esophageal varices (EV), hepatic encephalopathy (HE) and spontaneous bacterial peritonitis (SBP), who developed biloma and strictures after right hepatectomy, requiring stenting and sphincterotomy. A 9.0 cm segment 2 and 3 HA formed 56 days after MWA growing Morganella and Pseudomonas treated with 6 weeks cefepime and drain placement for 50 days. He had two more recurrences of HA.
Patient 2 is a 76-year-old male with HCV cirrhosis (Child B) complicated by HCC with MWA and transarterial radioembolization (TARE), ascites and portal vein thrombus (PVT) who developed ischemic hilar strictures and biloma after yttrium-90 TARE. A 7.3 cm segment 5 and 8 HA formed 12 days after MWA growing Klebsiella treated with 4 weeks ceftriaxone and metronidazole and drain placement for 84 days.
Patient 3 is a 72-year-old male with pancreatic adenocarcinoma and HCV cirrhosis (Child A) complicated by HCC and ascites who underwent Whipple procedure and developed biliary strictures after MWA. A 6.9 cm segment 5 HA formed 20 days after MWA growing Enterococcus and Streptococcus treated with 3 weeks moxifloxacin and drain placement for 50 days.
Patient 4 is a 70-year-old woman with HIV, cholangiocarcinoma and HCV cirrhosis (Child B) complicated by HCC with MWA and TACE, ascites, EV, HE, SBP and PVT who developed malignant strictures requiring stents and sphincterotomy. A 6.1 cm segment 6 HA formed 1230 days after MWA growing Klebsiella, Streptococcus and Parvinomas complicated by cholangitis and bacteremia treated with 10 weeks of antibiotics narrowed to ceftazidime-avibactam and needle aspiration.
All patients received the same perioperative antibiotic prophylaxis.
Discussion: This case series demonstrates the role prior biliary manipulation may play in increasing susceptibility to HA formation in HCC patients undergoing LT. Further investigation into rates of HA in patients without biliary manipulation, with other comorbidities, and those receiving alternative prophylaxis is warranted.
Disclosures:
Vinay Rao indicated no relevant financial relationships.
Salil Chowdhury indicated no relevant financial relationships.
Jonathan Gross indicated no relevant financial relationships.
Justin Bilello indicated no relevant financial relationships.
Beatriz Torre indicated no relevant financial relationships.
Dina Halegoua-DeMarzio: Pfizer – Advisory Committee/Board Member.
Vinay Rao, MD, Salil Chowdhury, MD, Jonathan Gross, MD, JD, Justin Bilello, MD, Beatriz Torre, MD, Dina Halegoua-DeMarzio, MD. P4014 - Hepatic Abscess Development Following Locoregional Therapy for Hepatocellular Carcinoma in Patients With Decompensated Cirrhosis & Prior Biliary Manipulation: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
