Tuesday Poster Session
Category: Colon
P3016 - Parkinson’s Disease Is Associated with Worse Outcomes in Ischemic Colitis: A Retrospective Nationwide Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- ET
Enmanuel Then
Universidad Iberoamericana
Gazcue, Distrito Nacional, Dominican Republic
Presenting Author(s)
Enmanuel Then, 1, Praneeth Bandaru, MD2, Saigopal R. Gujjula, 3, Hamsika Moparty, MD2, Herby Jeanty, MD2, Jamil Shah, MD2, Rajarajeshwari Ramachandran, MD2, Vinaya Gaduputi, MD4
1Universidad Iberoamericana, Gazcue, Distrito Nacional, Dominican Republic; 2Brooklyn Hospital Center, Brooklyn, NY; 3American University of Antigua, Coolidge, Saint John, Antigua and Barbuda; 4Blanchard Valley Health System, Findlay, OH
Introduction: Ischemic colitis (IC) is a disorder that occurs when the blood supply of the large intestine becomes compromised. Known risk factors for the development of ischemic colitis include congestive heart failure, atrial fibrillation, and chronic obstructive pulmonary disease, among others. The effect of neurologic conditions on the development of ischemic colitis has seldom been studied. Parkinson’s disease (PD) in particular, which is known to affect central dopinergic pathways, may play a role in clinical outcomes in patients with ischemic colitis.
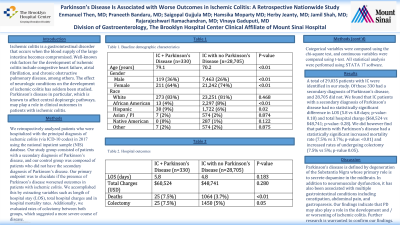
Methods: We retrospectively analyzed patients who were hospitalized with the principal diagnosis of ischemic colitis (via ICD-10 codes) in 2017 using the national inpatient sample (NIS) database. Our study group consisted of patients with a secondary diagnosis of Parkinson’s disease, and our control group was composed of patients who did not have the secondary diagnosis of Parkinson’s disease. Our primary endpoint was to elucidate if the presence of Parkinson’s disease worsened outcomes in patients with ischemic colitis. We accomplished this by extracting variables such as length of hospital stay (LOS), total hospital charges and in hospital mortality rates. Additionally we evaluated rates of colectomy between both groups, which suggested a more severe course of disease. Categorical variables were compared using the chi-square test, and continuous variables were compared using t-test. Statistical analysis were performed using STATA 17 software.
Results: A total of 29,035 patients with IC were identified in our study. Of these, 330 had a secondary diagnosis of PD, and 28,705 did not. We found that IC patients with a secondary diagnosis of PD had no statistically significant difference in LOS (5.8 vs 4.8 days; p-value: 0.18) and total hospital charge ($60,524 vs $48,741; p-value: 0.28). We did however find that patients with PD had a statistically significant increased mortality rate (7.5% vs 3.7%; p-value: < 0.01) and increased rates of undergoing colectomy (7.5% vs 5%; p-value 0.05).
Discussion: Parkinson’s disease is defined by degeneration of the Substantia Nigra whose primary role is to secrete dopamine in the midbrain. In addition to neuromuscular dysfunction, it has been associated with multiple gastrointestinal conditions including constipation, abdominal pain, and gastroparesis. Our findings indicate that PD may also play a role in the development and / or worsening of ischemic colitis. Further research is warranted to confirm our findings.

Disclosures:
Enmanuel Then, 1, Praneeth Bandaru, MD2, Saigopal R. Gujjula, 3, Hamsika Moparty, MD2, Herby Jeanty, MD2, Jamil Shah, MD2, Rajarajeshwari Ramachandran, MD2, Vinaya Gaduputi, MD4. P3016 - Parkinson’s Disease Is Associated with Worse Outcomes in Ischemic Colitis: A Retrospective Nationwide Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Universidad Iberoamericana, Gazcue, Distrito Nacional, Dominican Republic; 2Brooklyn Hospital Center, Brooklyn, NY; 3American University of Antigua, Coolidge, Saint John, Antigua and Barbuda; 4Blanchard Valley Health System, Findlay, OH
Introduction: Ischemic colitis (IC) is a disorder that occurs when the blood supply of the large intestine becomes compromised. Known risk factors for the development of ischemic colitis include congestive heart failure, atrial fibrillation, and chronic obstructive pulmonary disease, among others. The effect of neurologic conditions on the development of ischemic colitis has seldom been studied. Parkinson’s disease (PD) in particular, which is known to affect central dopinergic pathways, may play a role in clinical outcomes in patients with ischemic colitis.
Methods: We retrospectively analyzed patients who were hospitalized with the principal diagnosis of ischemic colitis (via ICD-10 codes) in 2017 using the national inpatient sample (NIS) database. Our study group consisted of patients with a secondary diagnosis of Parkinson’s disease, and our control group was composed of patients who did not have the secondary diagnosis of Parkinson’s disease. Our primary endpoint was to elucidate if the presence of Parkinson’s disease worsened outcomes in patients with ischemic colitis. We accomplished this by extracting variables such as length of hospital stay (LOS), total hospital charges and in hospital mortality rates. Additionally we evaluated rates of colectomy between both groups, which suggested a more severe course of disease. Categorical variables were compared using the chi-square test, and continuous variables were compared using t-test. Statistical analysis were performed using STATA 17 software.
Results: A total of 29,035 patients with IC were identified in our study. Of these, 330 had a secondary diagnosis of PD, and 28,705 did not. We found that IC patients with a secondary diagnosis of PD had no statistically significant difference in LOS (5.8 vs 4.8 days; p-value: 0.18) and total hospital charge ($60,524 vs $48,741; p-value: 0.28). We did however find that patients with PD had a statistically significant increased mortality rate (7.5% vs 3.7%; p-value: < 0.01) and increased rates of undergoing colectomy (7.5% vs 5%; p-value 0.05).
Discussion: Parkinson’s disease is defined by degeneration of the Substantia Nigra whose primary role is to secrete dopamine in the midbrain. In addition to neuromuscular dysfunction, it has been associated with multiple gastrointestinal conditions including constipation, abdominal pain, and gastroparesis. Our findings indicate that PD may also play a role in the development and / or worsening of ischemic colitis. Further research is warranted to confirm our findings.

Figure: Table 1. Baseline Demographic Characteristics
Table 2. Hospital Outcomes
Table 2. Hospital Outcomes
Disclosures:
Enmanuel Then indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Saigopal Gujjula indicated no relevant financial relationships.
Hamsika Moparty indicated no relevant financial relationships.
Herby Jeanty indicated no relevant financial relationships.
Jamil Shah indicated no relevant financial relationships.
Rajarajeshwari Ramachandran indicated no relevant financial relationships.
Vinaya Gaduputi indicated no relevant financial relationships.
Enmanuel Then, 1, Praneeth Bandaru, MD2, Saigopal R. Gujjula, 3, Hamsika Moparty, MD2, Herby Jeanty, MD2, Jamil Shah, MD2, Rajarajeshwari Ramachandran, MD2, Vinaya Gaduputi, MD4. P3016 - Parkinson’s Disease Is Associated with Worse Outcomes in Ischemic Colitis: A Retrospective Nationwide Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
