Tuesday Poster Session
Category: Colon
P3017 - Malnutrition Status Is an Independent Predictor for Worse Outcomes in Patients Hospitalized With Clostridioides difficile Infection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Abdelkader Chaar, MD
Yale University School of Medicine
New Haven, Connecticut
Presenting Author(s)
AbdelKader Chaar, MD1, Rabia Rizwan, MD1, Ahmad Nawaz, MD1, Shanti Patel, MD1, Tarek Aboursheid, MD2, Kanika Sehgal, MBBS3, Paul Feuerstadt, MD, FACG4
1Yale University School of Medicine, New Haven, CT; 2Ascension Saint Francis Hospital, Chicago, IL; 3Yale-New Haven Hospital, New Haven, CT; 4PACT Gastroenterology Center and Yale School of Medicine, Hamden, CT
Introduction: Malnutrition has major health implications for patients. However, the effect of malnutrition on patients with Clostridioides difficile infection (CDI) has not been properly evaluated. In this study, we examined this relationship utilizing a large national database within the United States.
Methods: Using the 2018 Nationwide Readmissions Database, we identified all adult patients who were discharged with a primary diagnosis of CDI. We then divided patients into 2 cohorts: those who had protein-calorie malnutrition (PCM) and those who did not (noPCM). PCM was defined as having a co-diagnosis of protein-calorie malnutrition of any degree. We investigated the effect of malnutrition on different CDI outcomes including 90-day readmission, 90-day CDI recurrence, hospital complications and healthcare utilization. Discharge-level weights were applied to provide national estimates.
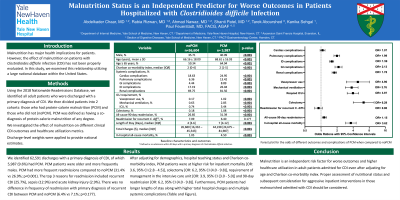
Results: We identified 62,591 discharges with a primary diagnosis of CDI, of which 5,987 (9.6%) had PCM. PCM patients were older (mean age 68.61 vs 66.16 years; p< 0.001) and more frequently males (40.1% vs 35.7%; p< 0.001). The overall 90-day CDI readmission rate was 27.3%; PCM had more frequent readmissions compared to noPCM (31.4% vs 26.9%; p< 0.001). The top 3 reasons for readmission included recurrent CDI (25.7%), sepsis (12.9%) and acute kidney injury (2.9%). There was no difference in frequency of readmission with primary diagnosis of recurrent CDI between PCM and noPCM (6.4% vs 7.1%; p=0.177). Using a multivariate analysis after adjusting for demographics, hospital teaching status and Charlson co-morbidity index, PCM patients were at higher risk for inpatient mortality [OR: 3.6, 95% CI (2.8 - 4.5); p< 0.001], colectomy [OR: 6.2, 95% CI (4.0 - 9.8); p< 0.001], requirement of management in the intensive care unit [OR: 3.9, 95% CI (3.0 - 5.0); p< 0.001] and 90-day readmission [OR: 6.2, 95% CI (4.0 - 9.8); p< 0.001]. Furthermore, PCM patients had longer lengths of stay along with higher total hospital charges and multiple systemic complications as compared with noPCM. (Table 1 and Figure 1).
Discussion: Malnutrition is an independent risk factor for worse outcomes and higher healthcare utilization in adult patients admitted for CDI even after adjusting for age and Charlson co-morbidity index. Proper assessment of nutritional status and subsequent consideration for aggressive inpatient interventions in those malnourished admitted with CDI should be considered.

Disclosures:
AbdelKader Chaar, MD1, Rabia Rizwan, MD1, Ahmad Nawaz, MD1, Shanti Patel, MD1, Tarek Aboursheid, MD2, Kanika Sehgal, MBBS3, Paul Feuerstadt, MD, FACG4. P3017 - Malnutrition Status Is an Independent Predictor for Worse Outcomes in Patients Hospitalized With Clostridioides difficile Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale University School of Medicine, New Haven, CT; 2Ascension Saint Francis Hospital, Chicago, IL; 3Yale-New Haven Hospital, New Haven, CT; 4PACT Gastroenterology Center and Yale School of Medicine, Hamden, CT
Introduction: Malnutrition has major health implications for patients. However, the effect of malnutrition on patients with Clostridioides difficile infection (CDI) has not been properly evaluated. In this study, we examined this relationship utilizing a large national database within the United States.
Methods: Using the 2018 Nationwide Readmissions Database, we identified all adult patients who were discharged with a primary diagnosis of CDI. We then divided patients into 2 cohorts: those who had protein-calorie malnutrition (PCM) and those who did not (noPCM). PCM was defined as having a co-diagnosis of protein-calorie malnutrition of any degree. We investigated the effect of malnutrition on different CDI outcomes including 90-day readmission, 90-day CDI recurrence, hospital complications and healthcare utilization. Discharge-level weights were applied to provide national estimates.
Results: We identified 62,591 discharges with a primary diagnosis of CDI, of which 5,987 (9.6%) had PCM. PCM patients were older (mean age 68.61 vs 66.16 years; p< 0.001) and more frequently males (40.1% vs 35.7%; p< 0.001). The overall 90-day CDI readmission rate was 27.3%; PCM had more frequent readmissions compared to noPCM (31.4% vs 26.9%; p< 0.001). The top 3 reasons for readmission included recurrent CDI (25.7%), sepsis (12.9%) and acute kidney injury (2.9%). There was no difference in frequency of readmission with primary diagnosis of recurrent CDI between PCM and noPCM (6.4% vs 7.1%; p=0.177). Using a multivariate analysis after adjusting for demographics, hospital teaching status and Charlson co-morbidity index, PCM patients were at higher risk for inpatient mortality [OR: 3.6, 95% CI (2.8 - 4.5); p< 0.001], colectomy [OR: 6.2, 95% CI (4.0 - 9.8); p< 0.001], requirement of management in the intensive care unit [OR: 3.9, 95% CI (3.0 - 5.0); p< 0.001] and 90-day readmission [OR: 6.2, 95% CI (4.0 - 9.8); p< 0.001]. Furthermore, PCM patients had longer lengths of stay along with higher total hospital charges and multiple systemic complications as compared with noPCM. (Table 1 and Figure 1).
Discussion: Malnutrition is an independent risk factor for worse outcomes and higher healthcare utilization in adult patients admitted for CDI even after adjusting for age and Charlson co-morbidity index. Proper assessment of nutritional status and subsequent consideration for aggressive inpatient interventions in those malnourished admitted with CDI should be considered.

Figure: Figure 1: Forest plot for the odds of different outcomes and complications of PCM when compared to noPCM (reference). Analysis was done using a multivariate logistic regression after adjusting for age, gender, race, hospital location and teaching status, insurance, median household income and Charlosn co-morbidity index.
Abbreviations: C. Diff: Clostridioides difficile, GI: Gastrointestinal; ID: Infectious Disease; ICU: Intensive Care Unit; PCM: Protein-Calorie Malnutrition
Abbreviations: C. Diff: Clostridioides difficile, GI: Gastrointestinal; ID: Infectious Disease; ICU: Intensive Care Unit; PCM: Protein-Calorie Malnutrition
Disclosures:
AbdelKader Chaar indicated no relevant financial relationships.
Rabia Rizwan indicated no relevant financial relationships.
Ahmad Nawaz indicated no relevant financial relationships.
Shanti Patel indicated no relevant financial relationships.
Tarek Aboursheid indicated no relevant financial relationships.
Kanika Sehgal indicated no relevant financial relationships.
Paul Feuerstadt: Ferring/Rebiotix, Inc. – Advisory Committee/Board Member, Consultant, Speakers Bureau. Merck & Co. – Consultant, Speakers Bureau. Seres Therapeutics – Advisory Committee/Board Member, Consultant, Speakers Bureau. Takeda Pharmaceuticals – Advisory Committee/Board Member, Consultant, Speakers Bureau.
AbdelKader Chaar, MD1, Rabia Rizwan, MD1, Ahmad Nawaz, MD1, Shanti Patel, MD1, Tarek Aboursheid, MD2, Kanika Sehgal, MBBS3, Paul Feuerstadt, MD, FACG4. P3017 - Malnutrition Status Is an Independent Predictor for Worse Outcomes in Patients Hospitalized With Clostridioides difficile Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
