Tuesday Poster Session
Category: Liver
P4020 - Not Your Typical Hematuria: A Rare Case of Hematuria Secondary to a Bleeding Varix
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Rafael Rivera Sepulveda, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Rafael Rivera Sepulveda, MD1, Chukwudumebi Uche, DO1, Omar Calderon, MD1, Jennifer L.. Seminerio, MD2
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida Health, Tampa, FL
Introduction: Bladder varices are an atypical cause of hematuria. Here we report a case of hematuria secondary to a bleeding bladder varix that was complicated by readmission for Spontaneous Bacterial Peritonitis (SBP).
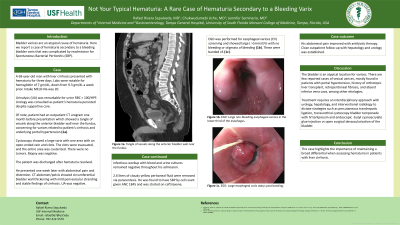
Case Description/Methods: A 69-year-old man with liver cirrhosis presented with hematuria for three days. Labs were notable for hemoglobin of 7 gm/dL, down from 9.3 gm/dL a week prior. Urinalysis (UA) was remarkable for urine RBC > 100/HPF. Intake MELD-Na was 20. Urology was consulted as patient’s hematuria persisted despite supportive care. Of note, patient had an outpatient CT urogram one month before presentation which showed a tangle of vessels along the anterior bladder wall near the fundus, concerning for varices related to patient’s cirrhosis and underlying portal hypertension (1a). Cystoscopy showed a large varix with one area with an open-ended vein and clots. The clots were removed, and the entire area was cauterized. There were no tumors. Biopsy was negative. The patient was discharged after hematuria resolved. He presented one week later with abdominal pain and distention. CT abdomen/pelvis showed circumferential bladder wall thickening with mild perivesicular stranding and stable findings of cirrhosis. UA was negative. Infectious workup with blood and urine cultures remained negative throughout his admission. 2.6 liters of cloudy yellow peritoneal fluid were removed via paracentesis. He was found to have SBP by cell count given ANC 1845 and was started on ceftriaxone. EGD was performed for esophageal varices (EV) screening and showed large ( >5mm) EVs with no bleeding or stigmata of bleeding (1b). These were banded x5 (1c). His abdominal pain improved with antibiotic therapy. Close outpatient follow-up with hepatology and urology was established.
Discussion: The bladder is an atypical location for varices. There are few reported cases of vesical varices, mostly found in patients with portal hypertension, history of orthotopic liver transplant, retroperitoneal fibrosis, and absent inferior vena cava, among other etiologies. Treatment requires an interdisciplinary approach with urology, hepatology, and interventional radiology to dictate strategies such as percutaneous transhepatic ligation, transurethral cystoscopy bladder tamponade with IV terlipressin and endoscopic -butyl cyanoacrylate glue injection vs open surgical devascularization of the bladder. This case highlights the importance of maintaining a broad differential when assessing hematuria in patients with liver cirrhosis.

Disclosures:
Rafael Rivera Sepulveda, MD1, Chukwudumebi Uche, DO1, Omar Calderon, MD1, Jennifer L.. Seminerio, MD2. P4020 - Not Your Typical Hematuria: A Rare Case of Hematuria Secondary to a Bleeding Varix, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida Health, Tampa, FL
Introduction: Bladder varices are an atypical cause of hematuria. Here we report a case of hematuria secondary to a bleeding bladder varix that was complicated by readmission for Spontaneous Bacterial Peritonitis (SBP).
Case Description/Methods: A 69-year-old man with liver cirrhosis presented with hematuria for three days. Labs were notable for hemoglobin of 7 gm/dL, down from 9.3 gm/dL a week prior. Urinalysis (UA) was remarkable for urine RBC > 100/HPF. Intake MELD-Na was 20. Urology was consulted as patient’s hematuria persisted despite supportive care. Of note, patient had an outpatient CT urogram one month before presentation which showed a tangle of vessels along the anterior bladder wall near the fundus, concerning for varices related to patient’s cirrhosis and underlying portal hypertension (1a). Cystoscopy showed a large varix with one area with an open-ended vein and clots. The clots were removed, and the entire area was cauterized. There were no tumors. Biopsy was negative. The patient was discharged after hematuria resolved. He presented one week later with abdominal pain and distention. CT abdomen/pelvis showed circumferential bladder wall thickening with mild perivesicular stranding and stable findings of cirrhosis. UA was negative. Infectious workup with blood and urine cultures remained negative throughout his admission. 2.6 liters of cloudy yellow peritoneal fluid were removed via paracentesis. He was found to have SBP by cell count given ANC 1845 and was started on ceftriaxone. EGD was performed for esophageal varices (EV) screening and showed large ( >5mm) EVs with no bleeding or stigmata of bleeding (1b). These were banded x5 (1c). His abdominal pain improved with antibiotic therapy. Close outpatient follow-up with hepatology and urology was established.
Discussion: The bladder is an atypical location for varices. There are few reported cases of vesical varices, mostly found in patients with portal hypertension, history of orthotopic liver transplant, retroperitoneal fibrosis, and absent inferior vena cava, among other etiologies. Treatment requires an interdisciplinary approach with urology, hepatology, and interventional radiology to dictate strategies such as percutaneous transhepatic ligation, transurethral cystoscopy bladder tamponade with IV terlipressin and endoscopic -butyl cyanoacrylate glue injection vs open surgical devascularization of the bladder. This case highlights the importance of maintaining a broad differential when assessing hematuria in patients with liver cirrhosis.

Figure: 1a. CT Abdomen/Pelvis: Tangle of vessels along the anterior bladder wall near the fundus.
1b. EGD: Large non-bleeding esophageal varices in lower third of the esophagus.
1c. EGD: Large esophageal varix status post banding.
1b. EGD: Large non-bleeding esophageal varices in lower third of the esophagus.
1c. EGD: Large esophageal varix status post banding.
Disclosures:
Rafael Rivera Sepulveda indicated no relevant financial relationships.
Chukwudumebi Uche indicated no relevant financial relationships.
Omar Calderon indicated no relevant financial relationships.
Jennifer Seminerio indicated no relevant financial relationships.
Rafael Rivera Sepulveda, MD1, Chukwudumebi Uche, DO1, Omar Calderon, MD1, Jennifer L.. Seminerio, MD2. P4020 - Not Your Typical Hematuria: A Rare Case of Hematuria Secondary to a Bleeding Varix, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
