Tuesday Poster Session
Category: Liver
P4023 - Challenges of Imaging Diagnosis in Budd-Chiari Syndrome
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- EB
Erin Biringen, MD
University of Arizona
Phoenix, AZ
Presenting Author(s)
Erin Biringen, MD1, Aaron Flegenheimer, MD2, Wesley A.. Robertson, MD, MPH, MPA3, Raha Sadjadi, MD3, Michael Fallon, MD4
1University of Arizona, Phoenix, AZ; 2University of Arizona College of Medicine, Gilbert, AZ; 3University of Arizona College of Medicine, Phoenix, AZ; 4Banner University Medical Center, Phoenix, AZ
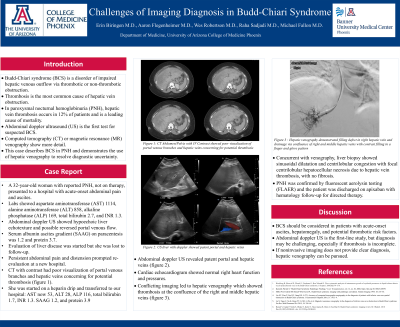
Introduction: Budd-Chiari syndrome (BCS) is a disorder of impaired hepatic venous outflow via thrombotic or non-thrombotic obstruction. Thrombosis is the most common cause of hepatic vein obstruction. In paroxysmal nocturnal hemoglobinuria (PNH), hepatic vein thrombosis occurs in 12% of patients and is a leading cause of mortality. Abdominal doppler ultrasound (US) is the first test for suspected BCS. Computed tomography (CT) or magnetic resonance (MR) venography show more detail. We present a case where conflicting imaging required hepatic venography to clench the diagnosis.
Case Description/Methods: A 32-year-old woman with reported PNH, not on therapy, presented to a hospital with acute-onset abdominal pain and ascites. Labs showed aspartate aminotransferase (AST) 1114, alanine aminotransferase (ALT) 858, alkaline phosphatase (ALP) 169, total bilirubin 2.7, and INR 1.3. Abdominal doppler US showed hypoechoic liver echotexture and possible reversed portal venous flow. Serum albumin ascites gradient (SAAG) was 1.2 and protein 3.7. Evaluation of liver disease was started but she was lost to follow-up.
Persistent abdominal pain and distension prompted re-evaluation at a new hospital. CT with contrast had poor visualization of portal venous branches and hepatic veins concerning for potential thrombosis. She was started on a heparin drip and transferred to our hospital. AST now 53, ALT 28, ALP 116, total bilirubin 1.7, INR 1.3. SAAG 1.2, and protein 3.9. Subsequent abdominal doppler US revealed patent portal and hepatic veins. Cardiac echocardiogram showed normal right heart function and pressures. The conflicting imaging led to hepatic venography which showed thrombosis at the confluence of the right and middle hepatic veins. Liver biopsy showed sinusoidal dilatation and centrilobular congestion with focal centrilobular hepatocellular necrosis due to hepatic vein thrombosis, with no fibrosis. PNH was confirmed by fluorescent aerolysin testing (FLAER). She was discharged on apixaban with hematology follow-up for directed therapy.
Discussion: BCS should be considered in patients with acute-onset ascites, hepatomegaly, and potential thrombotic risk factors. Abdominal doppler US is the first-line study, but diagnosis may be challenging, especially if thrombosis is incomplete. If noninvasive imaging does not provide clear diagnosis, hepatic venography can be pursued. This case describes BCS in PNH and demonstrates the use of hepatic venography to resolve diagnostic uncertainty.
Disclosures:
Erin Biringen, MD1, Aaron Flegenheimer, MD2, Wesley A.. Robertson, MD, MPH, MPA3, Raha Sadjadi, MD3, Michael Fallon, MD4. P4023 - Challenges of Imaging Diagnosis in Budd-Chiari Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona, Phoenix, AZ; 2University of Arizona College of Medicine, Gilbert, AZ; 3University of Arizona College of Medicine, Phoenix, AZ; 4Banner University Medical Center, Phoenix, AZ
Introduction: Budd-Chiari syndrome (BCS) is a disorder of impaired hepatic venous outflow via thrombotic or non-thrombotic obstruction. Thrombosis is the most common cause of hepatic vein obstruction. In paroxysmal nocturnal hemoglobinuria (PNH), hepatic vein thrombosis occurs in 12% of patients and is a leading cause of mortality. Abdominal doppler ultrasound (US) is the first test for suspected BCS. Computed tomography (CT) or magnetic resonance (MR) venography show more detail. We present a case where conflicting imaging required hepatic venography to clench the diagnosis.
Case Description/Methods: A 32-year-old woman with reported PNH, not on therapy, presented to a hospital with acute-onset abdominal pain and ascites. Labs showed aspartate aminotransferase (AST) 1114, alanine aminotransferase (ALT) 858, alkaline phosphatase (ALP) 169, total bilirubin 2.7, and INR 1.3. Abdominal doppler US showed hypoechoic liver echotexture and possible reversed portal venous flow. Serum albumin ascites gradient (SAAG) was 1.2 and protein 3.7. Evaluation of liver disease was started but she was lost to follow-up.
Persistent abdominal pain and distension prompted re-evaluation at a new hospital. CT with contrast had poor visualization of portal venous branches and hepatic veins concerning for potential thrombosis. She was started on a heparin drip and transferred to our hospital. AST now 53, ALT 28, ALP 116, total bilirubin 1.7, INR 1.3. SAAG 1.2, and protein 3.9. Subsequent abdominal doppler US revealed patent portal and hepatic veins. Cardiac echocardiogram showed normal right heart function and pressures. The conflicting imaging led to hepatic venography which showed thrombosis at the confluence of the right and middle hepatic veins. Liver biopsy showed sinusoidal dilatation and centrilobular congestion with focal centrilobular hepatocellular necrosis due to hepatic vein thrombosis, with no fibrosis. PNH was confirmed by fluorescent aerolysin testing (FLAER). She was discharged on apixaban with hematology follow-up for directed therapy.
Discussion: BCS should be considered in patients with acute-onset ascites, hepatomegaly, and potential thrombotic risk factors. Abdominal doppler US is the first-line study, but diagnosis may be challenging, especially if thrombosis is incomplete. If noninvasive imaging does not provide clear diagnosis, hepatic venography can be pursued. This case describes BCS in PNH and demonstrates the use of hepatic venography to resolve diagnostic uncertainty.
Disclosures:
Erin Biringen indicated no relevant financial relationships.
Aaron Flegenheimer indicated no relevant financial relationships.
Wesley Robertson indicated no relevant financial relationships.
Raha Sadjadi indicated no relevant financial relationships.
Michael Fallon indicated no relevant financial relationships.
Erin Biringen, MD1, Aaron Flegenheimer, MD2, Wesley A.. Robertson, MD, MPH, MPA3, Raha Sadjadi, MD3, Michael Fallon, MD4. P4023 - Challenges of Imaging Diagnosis in Budd-Chiari Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
