Tuesday Poster Session
Category: Obesity
P4027 - The Gender Gap in Bariatric Surgery: Outcomes and Utilization of Healthcare Services
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- CP
Chun-Wei Pan, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Chun-Wei Pan, MD1, Neethi Dasu, DO2, David Truscello, DO2, Muhammad Bilal Ibrahim, MD1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Jefferson Health, New Jersey, NJ
Introduction: As global obesity rates rise, so does the use of bariatric surgeries like Laparoscopic Gastric Bypass (LGB), Sleeve Gastrectomy (SG), and Laparoscopic Adjustable Band (LAGB) for weight loss. Although obesity affects both genders equally, more women undergo bariatric surgery. This study explores gender differences in bariatric surgeries outcomes and healthcare utilization.
Methods: We conducted a retrospective analysis using the National Inpatient Sample Database (NIS). Patients were identified based on procedure codes corresponding to LGB, SG, and LAGB, and further stratified by gender. Primary outcomes were all-cause mortality, with secondary outcomes including postoperative bleeding, infection, wound complication, respiratory failure), and healthcare utilization (mean length of stay (LOS) and total hospital charge (TOTCHG)).
Results:
Discussion: Using national data, we identified gender disparities in outcomes post-LGB, SG, and LAGB surgeries, with women showing more favorable results. This finding highlights the need to consider gender differences in clinical decision-making and patient counseling for bariatric surgeries. Further study is needed to understand the reasons behind these disparities.

Disclosures:
Chun-Wei Pan, MD1, Neethi Dasu, DO2, David Truscello, DO2, Muhammad Bilal Ibrahim, MD1. P4027 - The Gender Gap in Bariatric Surgery: Outcomes and Utilization of Healthcare Services, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Jefferson Health, New Jersey, NJ
Introduction: As global obesity rates rise, so does the use of bariatric surgeries like Laparoscopic Gastric Bypass (LGB), Sleeve Gastrectomy (SG), and Laparoscopic Adjustable Band (LAGB) for weight loss. Although obesity affects both genders equally, more women undergo bariatric surgery. This study explores gender differences in bariatric surgeries outcomes and healthcare utilization.
Methods: We conducted a retrospective analysis using the National Inpatient Sample Database (NIS). Patients were identified based on procedure codes corresponding to LGB, SG, and LAGB, and further stratified by gender. Primary outcomes were all-cause mortality, with secondary outcomes including postoperative bleeding, infection, wound complication, respiratory failure), and healthcare utilization (mean length of stay (LOS) and total hospital charge (TOTCHG)).
Results:
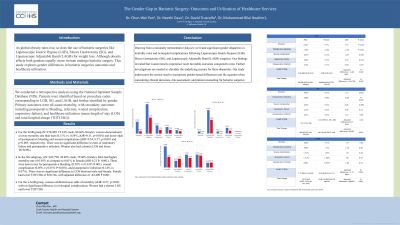
For the LGB group (N=270,480; 19.34% male, 80.66% female), women demonstrated a lower mortality rate than men (0.11% vs. 0.54%, aOR=0.31, p< 0.001) and lower odds of postoperative bleeding and wound complication (aOR=0.54, 0.57, p< 0.001 and p=0.005, respectively). There was no significant difference in rates of respiratory failure and postoperative infection. Women also had a shorter LOS and lower TOTCHG
In the SG subgroup, ((N=632,790; 20.40% male, 79.60% female). Men had higher mortality rate of 0.05% as compare to 0.01% in female (aOR 0.21 P: 0.001). There were lower rates for postoperative bleeding, (0.58% vs 0.34 P< 0.001), wound complication (0.05% vs 0.01% P< 0.001), and postoperative infection (0.14% vs 0.07%). There was no significant difference in LOS between male and female. Female had lower TOTCHG of $50,746, with adjusted difference of -$3,490 P 0.001.
For the LAGB group, women exhibited lower odds of mortality (aOR=0.57, p=0.02) with no significant difference in in-hospital complications. Women had a shorter LOS and lower TOTCHG
Discussion: Using national data, we identified gender disparities in outcomes post-LGB, SG, and LAGB surgeries, with women showing more favorable results. This finding highlights the need to consider gender differences in clinical decision-making and patient counseling for bariatric surgeries. Further study is needed to understand the reasons behind these disparities.

Figure: Comparison of in-hospital bariatric surgery outcomes; male versus female
Disclosures:
Chun-Wei Pan indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
David Truscello indicated no relevant financial relationships.
Muhammad Bilal Ibrahim indicated no relevant financial relationships.
Chun-Wei Pan, MD1, Neethi Dasu, DO2, David Truscello, DO2, Muhammad Bilal Ibrahim, MD1. P4027 - The Gender Gap in Bariatric Surgery: Outcomes and Utilization of Healthcare Services, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
