Tuesday Poster Session
Category: Colon
P3029 - Effectiveness and Safety of Thin vs Thick Cold Snare Polypectomy of Colorectal Polyps: A Systematic Review and Meta-analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- RK
Rishad Khan, MD
University of Toronto
Toronto, ON, Canada
Presenting Author(s)
Rishad Khan, MD1, Sunil Samnani, MD2, Marcus Vaska, MLIS2, Samir Grover, MD, MEd1, Catharine Walsh, MD, PhD1, Jeffrey Mosko, MD, MSc1, Michael Bourke, MBBS3, Steven Heitman, MD, MSc2, Nauzer Forbes, MD, MSc2
1University of Toronto, Toronto, ON, Canada; 2University of Calgary, Calgary, AB, Canada; 3Westmead Hospital, Westmead, New South Wales, Australia
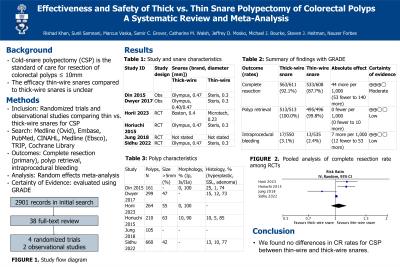
Introduction: Cold-snare polypectomy (CSP) is considered the standard of care for resection of colorectal polyps ≤ 10mm. Data on the efficacy of CSP performed with thin-wire snares compared to thick-wire snares are conflicting. We performed a meta-analysis comparing complete resection (CR) and adverse event rates of CSP using thin-wire and thick-wire snares.
Methods: Comparative studies of adult patients with ³1 colorectal polyp(s) £10 mm who underwent CSP with thin-wire or thick-wire snares were included. We collected data on study, patient, polyp, and snare characteristics. The primary outcome was CR rate. Secondary outcomes were polyp retrieval rate, intraprocedural bleeding, delayed post-polypectomy bleeding, deep mural injury or perforation, patient discomfort, total sedation, and procedure time. We used random-effects models to calculate risk ratios for outcomes. We performed risk of bias assessments, rated the certainty of evidence, and assessed publication bias for all studies.
Results: We included 4 randomized controlled trials (RCTs) and 2 observational studies including 1316 patients with 1679 polyps (826 thin-wire CSPs and 853 thick-wire CSPs). There was no significant difference between groups regarding CR rate for RCTs (92.1% versus 87.7%, RR 1.05, 95% CI 0.94-1.16) or observational studies (78.1% versus 79.6%, RR 1.03, 95% CI 0.99-1.08). There were no significant differences in polyp retrieval rate or intraprocedural bleeding. There were no cases of delayed bleeding or perforation.
Discussion: We found no differences in CR rates for CSP between thin-wire and thick-wire snares. CSP, regardless of snare type, is safe and effective for resection of small colorectal polyps.

Disclosures:
Rishad Khan, MD1, Sunil Samnani, MD2, Marcus Vaska, MLIS2, Samir Grover, MD, MEd1, Catharine Walsh, MD, PhD1, Jeffrey Mosko, MD, MSc1, Michael Bourke, MBBS3, Steven Heitman, MD, MSc2, Nauzer Forbes, MD, MSc2. P3029 - Effectiveness and Safety of Thin vs Thick Cold Snare Polypectomy of Colorectal Polyps: A Systematic Review and Meta-analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Toronto, Toronto, ON, Canada; 2University of Calgary, Calgary, AB, Canada; 3Westmead Hospital, Westmead, New South Wales, Australia
Introduction: Cold-snare polypectomy (CSP) is considered the standard of care for resection of colorectal polyps ≤ 10mm. Data on the efficacy of CSP performed with thin-wire snares compared to thick-wire snares are conflicting. We performed a meta-analysis comparing complete resection (CR) and adverse event rates of CSP using thin-wire and thick-wire snares.
Methods: Comparative studies of adult patients with ³1 colorectal polyp(s) £10 mm who underwent CSP with thin-wire or thick-wire snares were included. We collected data on study, patient, polyp, and snare characteristics. The primary outcome was CR rate. Secondary outcomes were polyp retrieval rate, intraprocedural bleeding, delayed post-polypectomy bleeding, deep mural injury or perforation, patient discomfort, total sedation, and procedure time. We used random-effects models to calculate risk ratios for outcomes. We performed risk of bias assessments, rated the certainty of evidence, and assessed publication bias for all studies.
Results: We included 4 randomized controlled trials (RCTs) and 2 observational studies including 1316 patients with 1679 polyps (826 thin-wire CSPs and 853 thick-wire CSPs). There was no significant difference between groups regarding CR rate for RCTs (92.1% versus 87.7%, RR 1.05, 95% CI 0.94-1.16) or observational studies (78.1% versus 79.6%, RR 1.03, 95% CI 0.99-1.08). There were no significant differences in polyp retrieval rate or intraprocedural bleeding. There were no cases of delayed bleeding or perforation.
Discussion: We found no differences in CR rates for CSP between thin-wire and thick-wire snares. CSP, regardless of snare type, is safe and effective for resection of small colorectal polyps.

Figure: Forest plots of primary and secondary outcomes. A: complete resection rate for randomized trials; B: complete resection rate for observational studies; C: polyp retrieval rate for randomized trials; D: polyp retrieval rate for observational studies; E: intraprocedural bleeding for randomized trials; F: intraprocedural bleeding for observational studies
Disclosures:
Rishad Khan indicated no relevant financial relationships.
Sunil Samnani indicated no relevant financial relationships.
Marcus Vaska indicated no relevant financial relationships.
Samir Grover: Abbvie – Grant/Research Support, Personal fees. Ferring Pharmaceuticals – Grant/Research Support, Personal fees. Janssen – Grant/Research Support. Takeda – Personal fees. Volo Healthcare – Stock-privately held company.
Catharine Walsh indicated no relevant financial relationships.
Jeffrey Mosko indicated no relevant financial relationships.
Michael Bourke: Boston Scientific – Grant/Research Support. Cook Medical – Grant/Research Support. Olympus – Grant/Research Support.
Steven Heitman indicated no relevant financial relationships.
Nauzer Forbes: AstraZeneca – Personal fees. Boston Scientific – Personal fees. Pentax Medical – Grant/Research Support, Personal fees.
Rishad Khan, MD1, Sunil Samnani, MD2, Marcus Vaska, MLIS2, Samir Grover, MD, MEd1, Catharine Walsh, MD, PhD1, Jeffrey Mosko, MD, MSc1, Michael Bourke, MBBS3, Steven Heitman, MD, MSc2, Nauzer Forbes, MD, MSc2. P3029 - Effectiveness and Safety of Thin vs Thick Cold Snare Polypectomy of Colorectal Polyps: A Systematic Review and Meta-analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
