Tuesday Poster Session
Category: Colon
P3033 - Impact of C. difficile Infection on Management of Cancer Patients With Diarrhea on Immune Checkpoint Inhibitors
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Patrick T. Magahis, BA
Weill Cornell Medicine
New York, NY
Presenting Author(s)
Patrick T.. Magahis, BA1, Deepika Satish, MD2, Monika Laszkowska, MD, MS2, David Faleck, MD2
1Weill Cornell Medicine, New York, NY; 2Memorial Sloan Kettering Cancer Center, New York, NY
Introduction: Immune checkpoint inhibitor-related enterocolitis (irEC) and infectious colitis often present with overlapping, nonspecific signs and symptoms. However, data are lacking on the rates and impact of C. difficile infection (CDI) on diarrhea course, severity, and the need for immunosuppressive therapy for irEC.
Methods: This retrospective cohort included all individuals undergoing immune checkpoint inhibitor (ICI) therapy and presenting with diarrhea who received CDI stool nucleic acid amplification testing at Memorial Sloan Kettering Cancer Center from 7/2015-7/2021. Patients with non-C. diff enteric infections were excluded. The primary outcome was the need for immunosuppressive therapy for suspected irEC according to CDI result status. Secondary outcomes included diarrhea severity and long-term clinical outcomes.
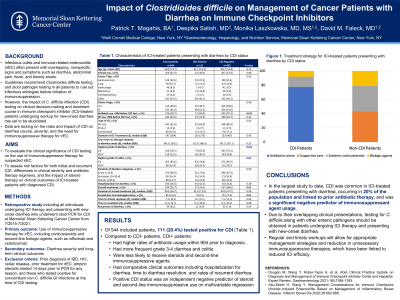
Results: A total of 441 patients were analyzed of whom 110 (25.0%) tested positive for CDI (Table 1). Patients with CDI had significantly higher rates of antibiotic usage within 90 days prior to diagnosis compared to those without CDI (63.6% vs. 47.7%, p< 0.01), while prior proton pump inhibitor (PPI) usage was not different. Patients with CDI had more frequent grade 3-4 diarrhea (32.7% vs. 19.6%, p=0.01). However, clinical outcomes including hospitalization for diarrhea (p=0.09), time to diarrhea resolution (p=0.93), and rates of recurrent diarrhea (p=0.09) were not significantly different between groups. CDI-positive patients were also less likely to receive steroids (12.7% vs. 23.0%, p=0.02) or steroids plus second-line immunosuppressive agents (7.3% vs. 16.3%, p=0.02) (Figure 1). A multivariable logistic regression model confirmed CDI positivity as being independently associated with a lower likelihood of steroid use (OR 0.42, p< 0.01) and second-line immunosuppressive therapy (OR 0.30, p=0.01).
Discussion: In the largest study to date, CDI was common in ICI-treated patients presenting with diarrhea, occurring in 25% of the population and linked to prior antibiotic therapy, and was a significant negative predictor of immunosuppressant agent usage. Due to their overlapping clinical presentations, testing for C. difficile along with other enteric pathogens should be obtained in patients undergoing ICI therapy and presenting with new-onset diarrhea. Regular and timely workups will allow for appropriate management strategies and reduction in unnecessary immunosuppressive therapies, which have been linked to reduced ICI efficacy.

Disclosures:
Patrick T.. Magahis, BA1, Deepika Satish, MD2, Monika Laszkowska, MD, MS2, David Faleck, MD2. P3033 - Impact of C. difficile Infection on Management of Cancer Patients With Diarrhea on Immune Checkpoint Inhibitors, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Weill Cornell Medicine, New York, NY; 2Memorial Sloan Kettering Cancer Center, New York, NY
Introduction: Immune checkpoint inhibitor-related enterocolitis (irEC) and infectious colitis often present with overlapping, nonspecific signs and symptoms. However, data are lacking on the rates and impact of C. difficile infection (CDI) on diarrhea course, severity, and the need for immunosuppressive therapy for irEC.
Methods: This retrospective cohort included all individuals undergoing immune checkpoint inhibitor (ICI) therapy and presenting with diarrhea who received CDI stool nucleic acid amplification testing at Memorial Sloan Kettering Cancer Center from 7/2015-7/2021. Patients with non-C. diff enteric infections were excluded. The primary outcome was the need for immunosuppressive therapy for suspected irEC according to CDI result status. Secondary outcomes included diarrhea severity and long-term clinical outcomes.
Results: A total of 441 patients were analyzed of whom 110 (25.0%) tested positive for CDI (Table 1). Patients with CDI had significantly higher rates of antibiotic usage within 90 days prior to diagnosis compared to those without CDI (63.6% vs. 47.7%, p< 0.01), while prior proton pump inhibitor (PPI) usage was not different. Patients with CDI had more frequent grade 3-4 diarrhea (32.7% vs. 19.6%, p=0.01). However, clinical outcomes including hospitalization for diarrhea (p=0.09), time to diarrhea resolution (p=0.93), and rates of recurrent diarrhea (p=0.09) were not significantly different between groups. CDI-positive patients were also less likely to receive steroids (12.7% vs. 23.0%, p=0.02) or steroids plus second-line immunosuppressive agents (7.3% vs. 16.3%, p=0.02) (Figure 1). A multivariable logistic regression model confirmed CDI positivity as being independently associated with a lower likelihood of steroid use (OR 0.42, p< 0.01) and second-line immunosuppressive therapy (OR 0.30, p=0.01).
Discussion: In the largest study to date, CDI was common in ICI-treated patients presenting with diarrhea, occurring in 25% of the population and linked to prior antibiotic therapy, and was a significant negative predictor of immunosuppressant agent usage. Due to their overlapping clinical presentations, testing for C. difficile along with other enteric pathogens should be obtained in patients undergoing ICI therapy and presenting with new-onset diarrhea. Regular and timely workups will allow for appropriate management strategies and reduction in unnecessary immunosuppressive therapies, which have been linked to reduced ICI efficacy.

Figure: Figure 1. Treatment strategy for ICI-treated patients presenting with diarrhea by CDI status.
Disclosures:
Patrick Magahis indicated no relevant financial relationships.
Deepika Satish indicated no relevant financial relationships.
Monika Laszkowska indicated no relevant financial relationships.
David Faleck: AzurRx – Consultant. Equillium – Consultant. Janssen – Consultant. Mallinckrodt Pharmaceuticals – Consultant. OnQuality Pharmaceuticals – Consultant.
Patrick T.. Magahis, BA1, Deepika Satish, MD2, Monika Laszkowska, MD, MS2, David Faleck, MD2. P3033 - Impact of C. difficile Infection on Management of Cancer Patients With Diarrhea on Immune Checkpoint Inhibitors, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
