Tuesday Poster Session
Category: Colon
P3034 - Neutropenic Enterocolitis in Children: A Review of the English Language Literature from 2000 Through 2022
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Grace Appah, MBChB
Achimota Hospital
Waterbury, CT
Presenting Author(s)
Grace Appah, MBChB1, Kwadwo A. Danso, MBChB2, Flora Danquah, MBChB3, Angela J. Boateng, MBBS4, Roberta Nartey, MBChB5, Fredrick Dapaah-Siakwan, MD6
1Achimota Hospital, Accra, Greater Accra, Ghana; 2Cape Coast Teaching Hospital, Cape Coast, Central, Ghana; 3University of North Carolina-Lineberger Comprehensive Cancer Center, Angier, NC; 4Kintegra Health Services, Gastonia, NC; 5Camkids Pediatrics PC, Cambria Heights, NY; 6Valley Children's Healthcare, Madera, CA
Introduction: Neutropenic enterocolitis (NE) is a rare but potentially life-threatening condition in cancer patients undergoing chemotherapy. There is a paucity of data on NE because of its rarity and lack of large-scale studies. We aimed to review pediatric NE within the literature to outline the disease course, management, and outcomes.
Methods: We searched PubMed and Google Scholar using the keywords ‘’pediatric’’, ''children'' ‘’neutropenic enterocolitis’’, and ''typhlitis''. We retrospectively reviewed case series published in English-Language, each with ≥3 patients from 2000 through 2022. Patients were cancer patients aged < 25 years undergoing chemotherapy or hematopoietic stem cell transplantation. We extracted the data from individual articles onto an Excel spreadsheet for further analysis. The outcomes of interest for the pooled data were clinical characteristics, hospital course and management, and mortality. Due to inconsistent reporting, the analysis was limited to reports that had complete information on each outcome of interest. Descriptive statistics were used to summarize the data
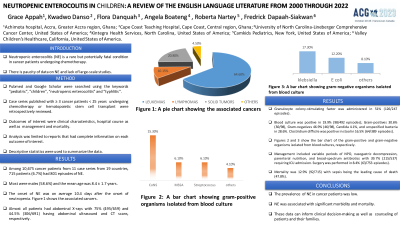
Results: Among 10,675 cancer patients from 11 case series from 19 countries, 715 patients (6.7%) had 801 episodes of NE. Most were male (58.6%) and the mean age was 8.4 ± 1.7 years. The associated cancers were: leukemias 64.6%, lymphomas 10.15, solid tumors 20.8%, and others 4.5%. The onset of NE was on average 10.4 days after the onset of neutropenia. Almost all patients had abdominal X-rays and 75% (495/659) and 44.5% (306/691) had abdominal ultrasound and CT scans, respectively. Granulocyte colony-stimulating factor was administered in 51% (126/247 episodes). Blood culture was positive in 19.9% (98/492 episodes) with Gram-negatives 46.9% (46/98: Klebsiella 17.3%; E coli 12.2%, others 8,1%), Gram-positives 30.6% (30/98; CONS 15.3%, MSSA 6.1%, Streptococcus 6.1%, others 4.1%), Candida 4.1%, and unspecified bacteria in 28.6%. Clostridium difficile was positive in stool in 16.5% (64/389 episodes). Surgery was performed in 8.4% (63/753 episodes). Management included variable periods of NPO, nasogastric decompression, parenteral nutrition, and broad-spectrum antibiotics with 39.7% (213/537) requiring ICU admission. Mortality was 12.9% (92/715) with sepsis being the leading cause of death (47.8%).
Discussion: The prevalence of NE in cancer patients was low but NE was associated with significant morbidity and mortality. These data can inform clinical decision-making and counseling of patients and their families.
Disclosures:
Grace Appah, MBChB1, Kwadwo A. Danso, MBChB2, Flora Danquah, MBChB3, Angela J. Boateng, MBBS4, Roberta Nartey, MBChB5, Fredrick Dapaah-Siakwan, MD6. P3034 - Neutropenic Enterocolitis in Children: A Review of the English Language Literature from 2000 Through 2022, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Achimota Hospital, Accra, Greater Accra, Ghana; 2Cape Coast Teaching Hospital, Cape Coast, Central, Ghana; 3University of North Carolina-Lineberger Comprehensive Cancer Center, Angier, NC; 4Kintegra Health Services, Gastonia, NC; 5Camkids Pediatrics PC, Cambria Heights, NY; 6Valley Children's Healthcare, Madera, CA
Introduction: Neutropenic enterocolitis (NE) is a rare but potentially life-threatening condition in cancer patients undergoing chemotherapy. There is a paucity of data on NE because of its rarity and lack of large-scale studies. We aimed to review pediatric NE within the literature to outline the disease course, management, and outcomes.
Methods: We searched PubMed and Google Scholar using the keywords ‘’pediatric’’, ''children'' ‘’neutropenic enterocolitis’’, and ''typhlitis''. We retrospectively reviewed case series published in English-Language, each with ≥3 patients from 2000 through 2022. Patients were cancer patients aged < 25 years undergoing chemotherapy or hematopoietic stem cell transplantation. We extracted the data from individual articles onto an Excel spreadsheet for further analysis. The outcomes of interest for the pooled data were clinical characteristics, hospital course and management, and mortality. Due to inconsistent reporting, the analysis was limited to reports that had complete information on each outcome of interest. Descriptive statistics were used to summarize the data
Results: Among 10,675 cancer patients from 11 case series from 19 countries, 715 patients (6.7%) had 801 episodes of NE. Most were male (58.6%) and the mean age was 8.4 ± 1.7 years. The associated cancers were: leukemias 64.6%, lymphomas 10.15, solid tumors 20.8%, and others 4.5%. The onset of NE was on average 10.4 days after the onset of neutropenia. Almost all patients had abdominal X-rays and 75% (495/659) and 44.5% (306/691) had abdominal ultrasound and CT scans, respectively. Granulocyte colony-stimulating factor was administered in 51% (126/247 episodes). Blood culture was positive in 19.9% (98/492 episodes) with Gram-negatives 46.9% (46/98: Klebsiella 17.3%; E coli 12.2%, others 8,1%), Gram-positives 30.6% (30/98; CONS 15.3%, MSSA 6.1%, Streptococcus 6.1%, others 4.1%), Candida 4.1%, and unspecified bacteria in 28.6%. Clostridium difficile was positive in stool in 16.5% (64/389 episodes). Surgery was performed in 8.4% (63/753 episodes). Management included variable periods of NPO, nasogastric decompression, parenteral nutrition, and broad-spectrum antibiotics with 39.7% (213/537) requiring ICU admission. Mortality was 12.9% (92/715) with sepsis being the leading cause of death (47.8%).
Discussion: The prevalence of NE in cancer patients was low but NE was associated with significant morbidity and mortality. These data can inform clinical decision-making and counseling of patients and their families.
Disclosures:
Grace Appah indicated no relevant financial relationships.
Kwadwo Danso indicated no relevant financial relationships.
Flora Danquah indicated no relevant financial relationships.
Angela Boateng indicated no relevant financial relationships.
Roberta Nartey indicated no relevant financial relationships.
Fredrick Dapaah-Siakwan indicated no relevant financial relationships.
Grace Appah, MBChB1, Kwadwo A. Danso, MBChB2, Flora Danquah, MBChB3, Angela J. Boateng, MBBS4, Roberta Nartey, MBChB5, Fredrick Dapaah-Siakwan, MD6. P3034 - Neutropenic Enterocolitis in Children: A Review of the English Language Literature from 2000 Through 2022, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
