Tuesday Poster Session
Category: Obesity
P4038 - Similar Protective Effects Between Common Types of Bariatric Surgery Against Obesity-Associated Cancer
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Vibhu Chittajallu, MD
Case Western Reserve University / University Hospitals
Cleveland, OH
Presenting Author(s)
Vibhu Chittajallu, MD1, Emad Mansoor, MD1, Jaime A. Perez, PhD2, C. Roberto Simons-Linares, MD3
1Case Western Reserve University / University Hospitals, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH
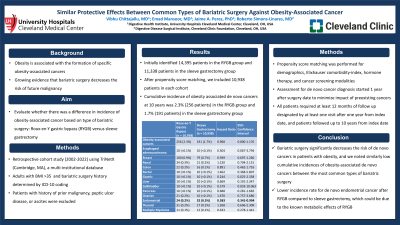
Introduction: Obesity is associated with the formation of specific obesity-associated cancers, and there is growing evidence that bariatric surgery decreases the risk of future malignancy. We aimed to further evaluate whether there was a difference in incidence of obesity-associated cancer based on type of bariatric surgery: Roux-en-Y gastric bypass (RYGB) versus sleeve gastrectomy.
Methods: This was a retrospective cohort study (2002-2022) using TriNetX (Cambridge, MA), a multi-institutional database from 82 US healthcare-organizations. Adults with BMI >35 were identified by ICD-10 coding. History of bariatric surgery (RYGB, sleeve gastrectomy) was determined by ICD-10 coding. Patients with history of prior malignancy, peptic ulcer disease, or ascites were excluded. Propensity score matching was performed for demographics, Elixhauser comorbidity-index, hormone therapy, and cancer screening modalities. We utilized the International Agency for Research on Cancer to determine cancers with sufficient evidence to be considered associated with obesity. Assessment for de novo cancer diagnosis started 1 year after time of RYGB or sleeve gastrectomy to minimize impact of preexisting cancers. All patients required at least 12 months of follow up designated by at least one visit after one year from index date, and patients followed up to 10 years from index date.
Results: We initially identified 14,395 patients in the RYGB group and 11,338 patients in the sleeve gastrectomy group. After propensity score matching, we included 10,938 patients in each cohort. The cumulative incidence of obesity associated de novo cancers at 10 years was 2.3% (256 patients) in the RYGB group and 1.7% (191 patients) in the sleeve gastrectomy group (HR 0.968 [CI 0.800-1.170]). Stratified analyses by specific cancer type revealed that RYGB group had lower incidence rates for de novo endometrial cancer (HR 0.583 [CI 0.341-0.994]) when compared to sleeve gastrectomy group.
Discussion: Bariatric surgery significantly decreases the risk of de novo cancers in patients with obesity, and we noted similarly low cumulative incidences of obesity-associated de novo cancers between the most common types of bariatric surgery. On stratified analyses, there was a lower incidence rate for de novo endometrial cancer after RYGB compared to sleeve gastrectomy, which could be due to the known metabolic effects of RYGB. This study supports the importance of treating obesity with bariatric surgery to reduce societal and economic burden of cancer.

Disclosures:
Vibhu Chittajallu, MD1, Emad Mansoor, MD1, Jaime A. Perez, PhD2, C. Roberto Simons-Linares, MD3. P4038 - Similar Protective Effects Between Common Types of Bariatric Surgery Against Obesity-Associated Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Case Western Reserve University / University Hospitals, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Obesity is associated with the formation of specific obesity-associated cancers, and there is growing evidence that bariatric surgery decreases the risk of future malignancy. We aimed to further evaluate whether there was a difference in incidence of obesity-associated cancer based on type of bariatric surgery: Roux-en-Y gastric bypass (RYGB) versus sleeve gastrectomy.
Methods: This was a retrospective cohort study (2002-2022) using TriNetX (Cambridge, MA), a multi-institutional database from 82 US healthcare-organizations. Adults with BMI >35 were identified by ICD-10 coding. History of bariatric surgery (RYGB, sleeve gastrectomy) was determined by ICD-10 coding. Patients with history of prior malignancy, peptic ulcer disease, or ascites were excluded. Propensity score matching was performed for demographics, Elixhauser comorbidity-index, hormone therapy, and cancer screening modalities. We utilized the International Agency for Research on Cancer to determine cancers with sufficient evidence to be considered associated with obesity. Assessment for de novo cancer diagnosis started 1 year after time of RYGB or sleeve gastrectomy to minimize impact of preexisting cancers. All patients required at least 12 months of follow up designated by at least one visit after one year from index date, and patients followed up to 10 years from index date.
Results: We initially identified 14,395 patients in the RYGB group and 11,338 patients in the sleeve gastrectomy group. After propensity score matching, we included 10,938 patients in each cohort. The cumulative incidence of obesity associated de novo cancers at 10 years was 2.3% (256 patients) in the RYGB group and 1.7% (191 patients) in the sleeve gastrectomy group (HR 0.968 [CI 0.800-1.170]). Stratified analyses by specific cancer type revealed that RYGB group had lower incidence rates for de novo endometrial cancer (HR 0.583 [CI 0.341-0.994]) when compared to sleeve gastrectomy group.
Discussion: Bariatric surgery significantly decreases the risk of de novo cancers in patients with obesity, and we noted similarly low cumulative incidences of obesity-associated de novo cancers between the most common types of bariatric surgery. On stratified analyses, there was a lower incidence rate for de novo endometrial cancer after RYGB compared to sleeve gastrectomy, which could be due to the known metabolic effects of RYGB. This study supports the importance of treating obesity with bariatric surgery to reduce societal and economic burden of cancer.

Figure: Obesity-Associated Cancer Incidence by Bariatric Surgery Type
Disclosures:
Vibhu Chittajallu indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
C. Roberto Simons-Linares indicated no relevant financial relationships.
Vibhu Chittajallu, MD1, Emad Mansoor, MD1, Jaime A. Perez, PhD2, C. Roberto Simons-Linares, MD3. P4038 - Similar Protective Effects Between Common Types of Bariatric Surgery Against Obesity-Associated Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
