Tuesday Poster Session
Category: Obesity
P4041 - Bariatric Surgery in Decompensated NASH Cirrhosis: Pushing the Limits
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sawsan Fathma, MD
Waterbury Hospital, Yale-Waterbury
Waterbury, CT
Presenting Author(s)
Sawsan Fathma, MD1, Daniel Kats, MD2, Albert Do, MD, MPH3
1Waterbury Hospital, Yale-Waterbury, Waterbury, CT; 2Yale-New Haven Hospital, New Haven, CT; 3Yale School of Medicine, New Haven, CT
Introduction: Metabolic bariatric surgery (MBS) is considered an elective surgery and so needs to be considered in context to patient risks and benefits yet can be substantially beneficial in carefully selected patients. We describe a patient with decompensated cirrhosis from nonalcoholic fatty liver disease (NAFLD) who successfully underwent sleeve gastrectomy (SG) with great benefit. We use this case to discuss physiological changes in cirrhosis and principals and tools for clinical surgical risk stratification in patients with liver disease.
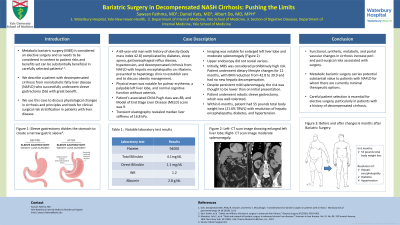
Case Description/Methods: A 69-year-old man with history of obesity (body mass index 42.8) complicated by diabetes, sleep apnea, gastroesophageal reflux disease, hypertension, and decompensated cirrhosis from NAFLD with hepatic encephalopathy on rifaximin, presented to hepatology clinic to establish care and to discuss obesity management. Physical exam was notable for palmar erythema, a palpable left liver lobe, and normal cognitive function without asterixis. Laboratory tests were notable for serum platelets 94, total bilirubin 4.1 mg/dL (direct 1.1), INR 1.2, and albumin 2.8 g/dL. His associated Child-Pugh class was 8B, and Model of End Stage Liver Disease (MELD) score was 9. Transient elastography revealed median liver stiffness of 16.8 kPa, MRI was notable for enlarged left liver lobe and moderate splenomegaly, and upper endoscopy did not reveal varices.
Initially, MBS was considered prohibitively high risk, but he underwent dietary lifestyle changes for 12 months, with BMI reduction to 39.9 and no new hepatic decompensation. Despite persistent mild splenomegaly, the risk was thought to be lower than on initial presentation, he then underwent robotic sleeve gastrectomy, which was well-tolerated. Within 6 months, he had 55 lbs total body weight loss (21.6% TBWL) with resolution of hepatic encephalopathy, diabetes, and hypertension.
Discussion: The functional synthetic, metabolic, and portal vascular changes in cirrhosis increase peri- and postsurgical risks associated with surgery. As a result, careful patient elective surgical selection is essential. Despite this, MBS carries potential substantial value to those with NAFLD, for whom there are no approved therapies available. We will discuss measures for risk mitigation including considerations for patient selection and clinical tools for risk stratification in cirrhosis, surgical approach, and perioperative optimization in decompensated cirrhosis.
Disclosures:
Sawsan Fathma, MD1, Daniel Kats, MD2, Albert Do, MD, MPH3. P4041 - Bariatric Surgery in Decompensated NASH Cirrhosis: Pushing the Limits, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Waterbury Hospital, Yale-Waterbury, Waterbury, CT; 2Yale-New Haven Hospital, New Haven, CT; 3Yale School of Medicine, New Haven, CT
Introduction: Metabolic bariatric surgery (MBS) is considered an elective surgery and so needs to be considered in context to patient risks and benefits yet can be substantially beneficial in carefully selected patients. We describe a patient with decompensated cirrhosis from nonalcoholic fatty liver disease (NAFLD) who successfully underwent sleeve gastrectomy (SG) with great benefit. We use this case to discuss physiological changes in cirrhosis and principals and tools for clinical surgical risk stratification in patients with liver disease.
Case Description/Methods: A 69-year-old man with history of obesity (body mass index 42.8) complicated by diabetes, sleep apnea, gastroesophageal reflux disease, hypertension, and decompensated cirrhosis from NAFLD with hepatic encephalopathy on rifaximin, presented to hepatology clinic to establish care and to discuss obesity management. Physical exam was notable for palmar erythema, a palpable left liver lobe, and normal cognitive function without asterixis. Laboratory tests were notable for serum platelets 94, total bilirubin 4.1 mg/dL (direct 1.1), INR 1.2, and albumin 2.8 g/dL. His associated Child-Pugh class was 8B, and Model of End Stage Liver Disease (MELD) score was 9. Transient elastography revealed median liver stiffness of 16.8 kPa, MRI was notable for enlarged left liver lobe and moderate splenomegaly, and upper endoscopy did not reveal varices.
Initially, MBS was considered prohibitively high risk, but he underwent dietary lifestyle changes for 12 months, with BMI reduction to 39.9 and no new hepatic decompensation. Despite persistent mild splenomegaly, the risk was thought to be lower than on initial presentation, he then underwent robotic sleeve gastrectomy, which was well-tolerated. Within 6 months, he had 55 lbs total body weight loss (21.6% TBWL) with resolution of hepatic encephalopathy, diabetes, and hypertension.
Discussion: The functional synthetic, metabolic, and portal vascular changes in cirrhosis increase peri- and postsurgical risks associated with surgery. As a result, careful patient elective surgical selection is essential. Despite this, MBS carries potential substantial value to those with NAFLD, for whom there are no approved therapies available. We will discuss measures for risk mitigation including considerations for patient selection and clinical tools for risk stratification in cirrhosis, surgical approach, and perioperative optimization in decompensated cirrhosis.
Disclosures:
Sawsan Fathma indicated no relevant financial relationships.
Daniel Kats indicated no relevant financial relationships.
Albert Do indicated no relevant financial relationships.
Sawsan Fathma, MD1, Daniel Kats, MD2, Albert Do, MD, MPH3. P4041 - Bariatric Surgery in Decompensated NASH Cirrhosis: Pushing the Limits, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
