Tuesday Poster Session
Category: Practice Management
P4054 - Probiotics for the Prevention and Treatment of COVID-19: Systematic Review and Meta-Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sophia Dar, MD
Northshore-Long Island Jewish Medical Center
Springfield , IL
Presenting Author(s)
Aruba Sohail, MBBS1, Huzaifa Ahmad Cheema, MBBS2, Maidah Mithani, MBBS1, Abia Shahid, MBBS2, Ahmad Nawaz, MBBS2, Sharjeel Ahmad, MD3, Sophia Haroon Dar, MD4, Rehmat Ullah Awan, MD5
1Dow University of Health Sciences, Karachi, Sindh, Pakistan; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3University of Illinois College of Medicine, Peoria, IL; 4Northshore-Long Island Jewish Medical Center, New York, NY; 5Ochsner Rush Medical Center, Meridian, MS
Introduction: Gut microbiome exerts an important role in immune system regulation, specifically in systemic diseases like COVID-19 viral illness. Hence, we conducted a meta-analysis to investigate the role of probiotics in preventing and treating COVID-19 infection.
Methods: We searched PubMed, Embase, the Cochrane Library and ClinicalTrials.gov from inception to 30 January 2023 for all eligible studies. We included all randomized controlled trials (RCTs) and comparative observational studies that investigated the efficacy of probiotics (irrespective of the regimen) for the treatment or prevention of COVID-19. The primary outcome was the risk of all-cause mortality, while the secondary outcomes included the rates of ICU admission, length of hospital stay, time to recovery, rate of no recovery. For studies that assessed the use of probiotics as a prophylactic measure against COVID-19, our outcome was the incidence of COVID-19 cases. We conducted our meta-analysis using RevMan 5.4 with risk ratio (RR) and mean difference (MD) as the effect measures. We stratified all our analyses according to the type of study (RCT vs. observational study).
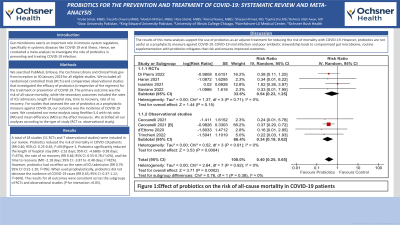
Results: A total of 18 studies (11 RCTs and 7 observational studies) were included in our review. Probiotics reduced the risk of mortality in COVID-19 patients (RR 0.40; 95% CI: 0.25-0.65, I2=0%)Figure-1. Probiotics significantly reduced the length of hospital stay (MD -2.52 days; 95% CI: -4.66 to -0.38 days; I2=67%), the rate of no recovery (RR 0.66; 95% CI: 0.55-0.78; I2=0%), and the time to recovery (MD -2.18 days; 95% CI: -3.87 to -0.48 days; I2=82%). However, probiotics had no effect on the rates of ICU admission (RR 0.79; 95% CI: 0.52-1.20; I2=0%). When used prophylactically, probiotics did not decrease the incidence of COVID-19 cases (RR 0.65; 95% CI: 0.37-1.12; I2=66%). The results for all outcomes were consistent across the subgroups of RCTs and observational studies (P for interaction >0.05).
Discussion: The results of this meta-analysis support the use of probiotics as an adjunct treatment for reducing the risk of mortality with COVID-19. However, probiotics are not useful as a prophylactic measure against COVID-19. COVID-19 viral infection and poor antibiotic stewardship leads to compromised gut microbiome, routine supplementation with probiotics mitigates that risk and ensures improved outcomes.

Disclosures:
Aruba Sohail, MBBS1, Huzaifa Ahmad Cheema, MBBS2, Maidah Mithani, MBBS1, Abia Shahid, MBBS2, Ahmad Nawaz, MBBS2, Sharjeel Ahmad, MD3, Sophia Haroon Dar, MD4, Rehmat Ullah Awan, MD5. P4054 - Probiotics for the Prevention and Treatment of COVID-19: Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Dow University of Health Sciences, Karachi, Sindh, Pakistan; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3University of Illinois College of Medicine, Peoria, IL; 4Northshore-Long Island Jewish Medical Center, New York, NY; 5Ochsner Rush Medical Center, Meridian, MS
Introduction: Gut microbiome exerts an important role in immune system regulation, specifically in systemic diseases like COVID-19 viral illness. Hence, we conducted a meta-analysis to investigate the role of probiotics in preventing and treating COVID-19 infection.
Methods: We searched PubMed, Embase, the Cochrane Library and ClinicalTrials.gov from inception to 30 January 2023 for all eligible studies. We included all randomized controlled trials (RCTs) and comparative observational studies that investigated the efficacy of probiotics (irrespective of the regimen) for the treatment or prevention of COVID-19. The primary outcome was the risk of all-cause mortality, while the secondary outcomes included the rates of ICU admission, length of hospital stay, time to recovery, rate of no recovery. For studies that assessed the use of probiotics as a prophylactic measure against COVID-19, our outcome was the incidence of COVID-19 cases. We conducted our meta-analysis using RevMan 5.4 with risk ratio (RR) and mean difference (MD) as the effect measures. We stratified all our analyses according to the type of study (RCT vs. observational study).
Results: A total of 18 studies (11 RCTs and 7 observational studies) were included in our review. Probiotics reduced the risk of mortality in COVID-19 patients (RR 0.40; 95% CI: 0.25-0.65, I2=0%)Figure-1. Probiotics significantly reduced the length of hospital stay (MD -2.52 days; 95% CI: -4.66 to -0.38 days; I2=67%), the rate of no recovery (RR 0.66; 95% CI: 0.55-0.78; I2=0%), and the time to recovery (MD -2.18 days; 95% CI: -3.87 to -0.48 days; I2=82%). However, probiotics had no effect on the rates of ICU admission (RR 0.79; 95% CI: 0.52-1.20; I2=0%). When used prophylactically, probiotics did not decrease the incidence of COVID-19 cases (RR 0.65; 95% CI: 0.37-1.12; I2=66%). The results for all outcomes were consistent across the subgroups of RCTs and observational studies (P for interaction >0.05).
Discussion: The results of this meta-analysis support the use of probiotics as an adjunct treatment for reducing the risk of mortality with COVID-19. However, probiotics are not useful as a prophylactic measure against COVID-19. COVID-19 viral infection and poor antibiotic stewardship leads to compromised gut microbiome, routine supplementation with probiotics mitigates that risk and ensures improved outcomes.

Figure: Effect of probiotics on the risk of all-cause mortality in COVID-19 patients.
Disclosures:
Aruba Sohail indicated no relevant financial relationships.
Huzaifa Ahmad Cheema indicated no relevant financial relationships.
Maidah Mithani indicated no relevant financial relationships.
Abia Shahid indicated no relevant financial relationships.
Ahmad Nawaz indicated no relevant financial relationships.
Sharjeel Ahmad indicated no relevant financial relationships.
Sophia Haroon Dar indicated no relevant financial relationships.
Rehmat Ullah Awan indicated no relevant financial relationships.
Aruba Sohail, MBBS1, Huzaifa Ahmad Cheema, MBBS2, Maidah Mithani, MBBS1, Abia Shahid, MBBS2, Ahmad Nawaz, MBBS2, Sharjeel Ahmad, MD3, Sophia Haroon Dar, MD4, Rehmat Ullah Awan, MD5. P4054 - Probiotics for the Prevention and Treatment of COVID-19: Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
