Tuesday Poster Session
Category: Colon
P3054 - A Not so Fun Guy: A Curious Case of Fungal Colitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Anthony M. Rainho, MD
University of Virginia
Charlottesville, VA
Presenting Author(s)
Award: Presidential Poster Award
Anthony M. Rainho, MD, Rebecca M. Haug, MD, Vanessa M. Shami, MD, Andrew P. Copland, MD, Shyam Raghavan, MD, Amanda Gibbs, MD
University of Virginia, Charlottesville, VA
Introduction: Infectious colitis commonly presents with fever and diarrhea. Immunocompromised populations are at higher risk of developing infectious colitis, with viral, opportunistic bacterial, and parasitic infections often ruled out as part of the initial evaluation. Fungal etiologies, however, are often overlooked, and co-infection may not be considered. We present a rare case of an immunocompromised patient following a kidney transplant who failed to progress on typical treatment for confirmed Clostridium difficile colitis and was ultimately diagnosed with fungal colitis after biopsies revealed Histoplasma capsulatum.
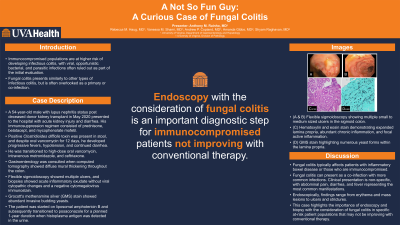
Case Description/Methods: A 54-year-old male with a history of lupus nephritis status post deceased donor kidney transplant in May 2020 presented to the hospital with acute kidney injury and diarrhea. His immunosuppression regimen consisted of prednisone, belatacept, and mycophenolate mofetil. Workup revealed positive Clostridium difficile toxin production in his stool, and he was treated with oral vancomycin for 12 days. He developed progressive fevers, hypotension, and continued diarrhea, so transitioned to high-dose oral vancomycin, intravenous metronidazole, and ceftriaxone. Gastroenterology was consulted when computed tomography showed diffuse mural thickening throughout the colon. Given the patient’s immunocompromised status, a flexible sigmoidoscopy was performed and showed multiple small to medium ulcers. Biopsies showed acute inflammatory exudate without viral cytopathic changes and a negative CMV immunostain. Given the concern for atypical infection, a Grocott's methenamine silver (GMS) stain was performed and showed abundant invasive budding yeasts. The patient was started on liposomal amphotericin B and subsequently transitioned to posaconazole for a planned 1-year duration when histoplasma antigen was detected in the urine.
Discussion: Fungal colitis typically affects patients with inflammatory bowel disease or those who are immunocompromised and can present as a co-infection with other, more common infections. Clinical presentation is non-specific, with abdominal pain, diarrhea, and fever representing the most common manifestations. Endoscopically, findings can range from erythema and mass lesions to ulcers and strictures. This case highlights the importance of endoscopy and biopsy with the consideration of fungal colitis in specific at-risk patient populations who may not be improving with conventional therapy.

Disclosures:
Anthony M. Rainho, MD, Rebecca M. Haug, MD, Vanessa M. Shami, MD, Andrew P. Copland, MD, Shyam Raghavan, MD, Amanda Gibbs, MD. P3054 - A Not so Fun Guy: A Curious Case of Fungal Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Anthony M. Rainho, MD, Rebecca M. Haug, MD, Vanessa M. Shami, MD, Andrew P. Copland, MD, Shyam Raghavan, MD, Amanda Gibbs, MD
University of Virginia, Charlottesville, VA
Introduction: Infectious colitis commonly presents with fever and diarrhea. Immunocompromised populations are at higher risk of developing infectious colitis, with viral, opportunistic bacterial, and parasitic infections often ruled out as part of the initial evaluation. Fungal etiologies, however, are often overlooked, and co-infection may not be considered. We present a rare case of an immunocompromised patient following a kidney transplant who failed to progress on typical treatment for confirmed Clostridium difficile colitis and was ultimately diagnosed with fungal colitis after biopsies revealed Histoplasma capsulatum.
Case Description/Methods: A 54-year-old male with a history of lupus nephritis status post deceased donor kidney transplant in May 2020 presented to the hospital with acute kidney injury and diarrhea. His immunosuppression regimen consisted of prednisone, belatacept, and mycophenolate mofetil. Workup revealed positive Clostridium difficile toxin production in his stool, and he was treated with oral vancomycin for 12 days. He developed progressive fevers, hypotension, and continued diarrhea, so transitioned to high-dose oral vancomycin, intravenous metronidazole, and ceftriaxone. Gastroenterology was consulted when computed tomography showed diffuse mural thickening throughout the colon. Given the patient’s immunocompromised status, a flexible sigmoidoscopy was performed and showed multiple small to medium ulcers. Biopsies showed acute inflammatory exudate without viral cytopathic changes and a negative CMV immunostain. Given the concern for atypical infection, a Grocott's methenamine silver (GMS) stain was performed and showed abundant invasive budding yeasts. The patient was started on liposomal amphotericin B and subsequently transitioned to posaconazole for a planned 1-year duration when histoplasma antigen was detected in the urine.
Discussion: Fungal colitis typically affects patients with inflammatory bowel disease or those who are immunocompromised and can present as a co-infection with other, more common infections. Clinical presentation is non-specific, with abdominal pain, diarrhea, and fever representing the most common manifestations. Endoscopically, findings can range from erythema and mass lesions to ulcers and strictures. This case highlights the importance of endoscopy and biopsy with the consideration of fungal colitis in specific at-risk patient populations who may not be improving with conventional therapy.

Figure: (A & B) Flexible sigmoidoscopy showing multiple small to medium sized ulcers in the sigmoid colon. (C) H&E stain demonstrating expanded lamina propria, abundant chronic inflammation, and focal active inflammation. (D) GMS stain highlighting numerous yeast forms within the lamina propria.
Disclosures:
Anthony Rainho indicated no relevant financial relationships.
Rebecca Haug indicated no relevant financial relationships.
Vanessa Shami: Boston Scientific – Consultant. Cook Medical – Consultant. Olympus America – Consultant.
Andrew Copland indicated no relevant financial relationships.
Shyam Raghavan indicated no relevant financial relationships.
Amanda Gibbs indicated no relevant financial relationships.
Anthony M. Rainho, MD, Rebecca M. Haug, MD, Vanessa M. Shami, MD, Andrew P. Copland, MD, Shyam Raghavan, MD, Amanda Gibbs, MD. P3054 - A Not so Fun Guy: A Curious Case of Fungal Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

