Tuesday Poster Session
Category: Practice Management
P4059 - Something Doesn't FIT: Reducing Lab-Rejected FIT Specimens at the Veteran Affairs Medical Center
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Elizabeth A. Rowland, MD, MBA
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Elizabeth A. Rowland, MD, MBA1, Wesley A.. Robertson, MD, MPH, MPA1, Mohamed Abdelhabib, MD1, Jolyn Moeller, RN, ACNS-BC2, Melinda Somoza, MD2, Freya Spielberg, MD, MPH2, Anthony Millett, MST2, Alvin G. Wong, MD2
1University of Arizona College of Medicine, Phoenix, AZ; 2Phoenix VA Health Care System, Phoenix, AZ
Introduction: Colorectal cancer (CRC) contributes to significant mortality in the United States, ranking second for cancer-related deaths. The American College of Gastroenterology (ACG) recommends colonoscopy or FIT as the primary CRC screening method. FIT detects CRC with 91% sensitivity and 90% specificity. Repeated annual FIT leads to an 80% CRC detection rate. FIT testing requires patients to collect and submit a stool sample from home using an at-home kit. An initial review of data at the Phoenix Veterans Affairs Medical Center found that, in February 2023 alone, 18% of FIT specimens returned to lab were rejected. A quality improvement task force was convened to further investigate this discrepancy and develop strategies to reduce rejected FIT specimens.
Methods: A representative sample of key stakeholders were engaged to determine procedural inadequacies. This cohort includes laboratory staff, who determine from eligibility criteria if a specimen is acceptable; the primary care provider who orders testing and advises patients; and the patient population, who perform the majority of FIT process.
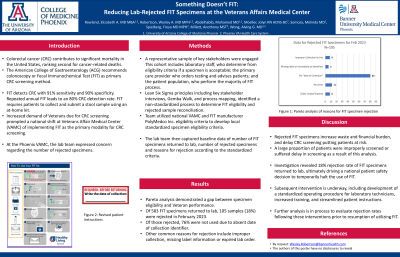
Results: A Gemba walk revealed a non-standardized process to determine specimen rejection and underlying cause of specimen rejection. Pareto analysis demonstrated a gap between specimen eligibility criteria and Veteran performance. Of the 105 rejected samples in February 2023, 80 samples (76%) were not collected due to absent date of collection identifier. Other common reasons for rejection include improper collection, missing label information, or expired date of submission.
As a result of this finding, executive leadership intervened and temporarily halted ordering of FIT testing pending further process evaluation and demonstrated improvement.
Discussion: Rejected FIT specimens increase waste and financial burden, and delay CRC screening rates putting patients at risk. A large proportion of patients were discovered to be improperly screened as a result of this analysis, and FIT testing has been temporarily halted to ensure patient safety. Study findings have informed a national effort to improve FIT testing procedures at the VA Health System. Subsequent intervention is currently underway, which includes development of a standardized operating procedure for laboratory technicians, increased training, and streamlined patient instructions. Further analysis is in process to evaluate rejection rates following this intervention.
Disclosures:
Elizabeth A. Rowland, MD, MBA1, Wesley A.. Robertson, MD, MPH, MPA1, Mohamed Abdelhabib, MD1, Jolyn Moeller, RN, ACNS-BC2, Melinda Somoza, MD2, Freya Spielberg, MD, MPH2, Anthony Millett, MST2, Alvin G. Wong, MD2. P4059 - Something Doesn't FIT: Reducing Lab-Rejected FIT Specimens at the Veteran Affairs Medical Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2Phoenix VA Health Care System, Phoenix, AZ
Introduction: Colorectal cancer (CRC) contributes to significant mortality in the United States, ranking second for cancer-related deaths. The American College of Gastroenterology (ACG) recommends colonoscopy or FIT as the primary CRC screening method. FIT detects CRC with 91% sensitivity and 90% specificity. Repeated annual FIT leads to an 80% CRC detection rate. FIT testing requires patients to collect and submit a stool sample from home using an at-home kit. An initial review of data at the Phoenix Veterans Affairs Medical Center found that, in February 2023 alone, 18% of FIT specimens returned to lab were rejected. A quality improvement task force was convened to further investigate this discrepancy and develop strategies to reduce rejected FIT specimens.
Methods: A representative sample of key stakeholders were engaged to determine procedural inadequacies. This cohort includes laboratory staff, who determine from eligibility criteria if a specimen is acceptable; the primary care provider who orders testing and advises patients; and the patient population, who perform the majority of FIT process.
Results: A Gemba walk revealed a non-standardized process to determine specimen rejection and underlying cause of specimen rejection. Pareto analysis demonstrated a gap between specimen eligibility criteria and Veteran performance. Of the 105 rejected samples in February 2023, 80 samples (76%) were not collected due to absent date of collection identifier. Other common reasons for rejection include improper collection, missing label information, or expired date of submission.
As a result of this finding, executive leadership intervened and temporarily halted ordering of FIT testing pending further process evaluation and demonstrated improvement.
Discussion: Rejected FIT specimens increase waste and financial burden, and delay CRC screening rates putting patients at risk. A large proportion of patients were discovered to be improperly screened as a result of this analysis, and FIT testing has been temporarily halted to ensure patient safety. Study findings have informed a national effort to improve FIT testing procedures at the VA Health System. Subsequent intervention is currently underway, which includes development of a standardized operating procedure for laboratory technicians, increased training, and streamlined patient instructions. Further analysis is in process to evaluate rejection rates following this intervention.
Disclosures:
Elizabeth Rowland indicated no relevant financial relationships.
Wesley Robertson indicated no relevant financial relationships.
Mohamed Abdelhabib indicated no relevant financial relationships.
Jolyn Moeller indicated no relevant financial relationships.
Melinda Somoza indicated no relevant financial relationships.
Freya Spielberg indicated no relevant financial relationships.
Anthony Millett indicated no relevant financial relationships.
Alvin Wong indicated no relevant financial relationships.
Elizabeth A. Rowland, MD, MBA1, Wesley A.. Robertson, MD, MPH, MPA1, Mohamed Abdelhabib, MD1, Jolyn Moeller, RN, ACNS-BC2, Melinda Somoza, MD2, Freya Spielberg, MD, MPH2, Anthony Millett, MST2, Alvin G. Wong, MD2. P4059 - Something Doesn't FIT: Reducing Lab-Rejected FIT Specimens at the Veteran Affairs Medical Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
