Tuesday Poster Session
Category: Practice Management
P4061 - The Hepatology-Addiction-Internal Medicine Co-Localization Model: An Innovative Approach to Achieving Treatment Adherence and Sustained Virologic Response in Psychiatric Patients Infected with Hepatitis C Virus
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Clive J. Miranda, DO, MS
University at Buffalo
Buffalo, NY
Presenting Author(s)
Clive J. Miranda, DO, MS, Alexander M. Carlson, DO, Naren S. Nallapeta, MBBS, Slah Khan, MPH, Yousaf Saeed, MD, Sawyer J. Bawek, DO, Anthony D. Martinez, MD
University at Buffalo, Buffalo, NY
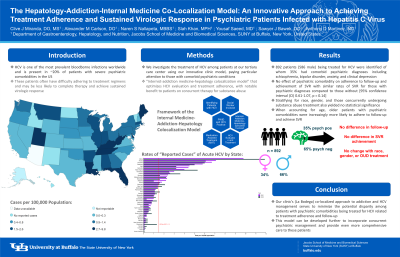
Introduction: Hepatitis C virus (HCV) is one of the most prevalent bloodborne infections worldwide and is present in ~20% of patients with severe psychiatric comorbidities in the United States. These patients often have difficulty adhering to treatment regimens and may be less likely to complete therapy and achieve sustained virologic response (SVR). Furthermore, concomitant substance abuse and addictive disorders could potentially impact treatment outcomes and clinical follow-up. We investigate the treatment of HCV among patients at our tertiary care center using our innovative clinic model, paying particular attention to those with comorbid psychiatric conditions.
Methods: A retrospective chart review of the electronic medical record at our Hepatology clinic – La Bodega – was conducted from 2014 to 2021. Data collected included age, gender, race, concurrent treatment for substance abuse, and psychiatric comorbidities. Logistic regression models were created to assess for statistical significance between the presence of psychiatric comorbidities and adherence to follow-up. Our institution utilizes an “internist-addiction medicine-hepatology colocalization model” that optimizes HCV evaluation and treatment adherence, with notable benefit to patients on concurrent therapy for substance abuse.
Results: A total of 892 patients (586 male) being treated for HCV were identified of whom 35% had comorbid psychiatric diagnoses including schizophrenia, bipolar disorder, anxiety, and clinical depression. There was no effect of psychiatric comorbidity on adherence to follow-up and achievement of SVR with similar rates of SVR for those with psychiatric diagnoses compared to those without [95% confidence interval (CI) 0.61-1.07, p = 0.14]. Stratifying for race, gender, and those concurrently undergoing substance abuse treatment also yielded no statistical significance. However, when accounting for age, older patients with psychiatric comorbidities were increasingly more likely to adhere to follow-up and achieve SVR.
Discussion: Our clinic’s (La Bodega) co-localized approach to addiction and HCV management serves to minimize the potential disparity among patients with psychiatric comorbidities being treated for HCV related to treatment adherence and follow-up. This model can be developed further to incorporate concurrent psychiatric management and provide even more comprehensive care to these patients.
Disclosures:
Clive J. Miranda, DO, MS, Alexander M. Carlson, DO, Naren S. Nallapeta, MBBS, Slah Khan, MPH, Yousaf Saeed, MD, Sawyer J. Bawek, DO, Anthony D. Martinez, MD. P4061 - The Hepatology-Addiction-Internal Medicine Co-Localization Model: An Innovative Approach to Achieving Treatment Adherence and Sustained Virologic Response in Psychiatric Patients Infected with Hepatitis C Virus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Hepatitis C virus (HCV) is one of the most prevalent bloodborne infections worldwide and is present in ~20% of patients with severe psychiatric comorbidities in the United States. These patients often have difficulty adhering to treatment regimens and may be less likely to complete therapy and achieve sustained virologic response (SVR). Furthermore, concomitant substance abuse and addictive disorders could potentially impact treatment outcomes and clinical follow-up. We investigate the treatment of HCV among patients at our tertiary care center using our innovative clinic model, paying particular attention to those with comorbid psychiatric conditions.
Methods: A retrospective chart review of the electronic medical record at our Hepatology clinic – La Bodega – was conducted from 2014 to 2021. Data collected included age, gender, race, concurrent treatment for substance abuse, and psychiatric comorbidities. Logistic regression models were created to assess for statistical significance between the presence of psychiatric comorbidities and adherence to follow-up. Our institution utilizes an “internist-addiction medicine-hepatology colocalization model” that optimizes HCV evaluation and treatment adherence, with notable benefit to patients on concurrent therapy for substance abuse.
Results: A total of 892 patients (586 male) being treated for HCV were identified of whom 35% had comorbid psychiatric diagnoses including schizophrenia, bipolar disorder, anxiety, and clinical depression. There was no effect of psychiatric comorbidity on adherence to follow-up and achievement of SVR with similar rates of SVR for those with psychiatric diagnoses compared to those without [95% confidence interval (CI) 0.61-1.07, p = 0.14]. Stratifying for race, gender, and those concurrently undergoing substance abuse treatment also yielded no statistical significance. However, when accounting for age, older patients with psychiatric comorbidities were increasingly more likely to adhere to follow-up and achieve SVR.
Discussion: Our clinic’s (La Bodega) co-localized approach to addiction and HCV management serves to minimize the potential disparity among patients with psychiatric comorbidities being treated for HCV related to treatment adherence and follow-up. This model can be developed further to incorporate concurrent psychiatric management and provide even more comprehensive care to these patients.
Disclosures:
Clive Miranda indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Naren Nallapeta indicated no relevant financial relationships.
Slah Khan indicated no relevant financial relationships.
Yousaf Saeed indicated no relevant financial relationships.
Sawyer Bawek indicated no relevant financial relationships.
Anthony Martinez indicated no relevant financial relationships.
Clive J. Miranda, DO, MS, Alexander M. Carlson, DO, Naren S. Nallapeta, MBBS, Slah Khan, MPH, Yousaf Saeed, MD, Sawyer J. Bawek, DO, Anthony D. Martinez, MD. P4061 - The Hepatology-Addiction-Internal Medicine Co-Localization Model: An Innovative Approach to Achieving Treatment Adherence and Sustained Virologic Response in Psychiatric Patients Infected with Hepatitis C Virus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
