Tuesday Poster Session
Category: Practice Management
P4078 - Development of a Clinical Nutrition Elective for an Internal Medicine Residency Program
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Michael Delicce, MD
Cleveland Clinic
Cleveland, Ohio
Presenting Author(s)
Michael Delicce, MD, Mary Rath, RD, CNSC, LD, Mattie White, MD, Jason Nasser, MD, Renee Welsh, MS, RD, LD, CNSC, Andrew Ford, MD, Puneet Dhillon, DO, Samia Mazumder, MD, Andrea Jevenn, MEd, RD, LD, CNSC, Donald Kirby, MD, FACG
Cleveland Clinic, Cleveland, OH
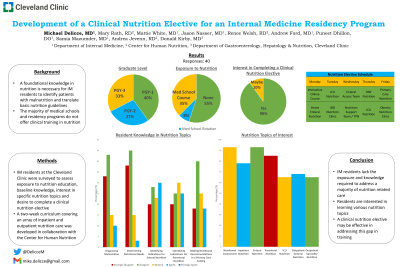
Introduction: A foundational knowledge in nutrition is necessary for internal medicine (IM) residents to identify patients with malnutrition and translate basic nutrition guidelines to improve patient care. However, the majority of medical schools and residency programs do not offer clinical training in nutrition. Therefore, it is imperative that residents have nutrition education incorporated into their training.
Methods: IM residents at our institution were surveyed to assess exposure to nutrition education, baseline knowledge in areas of nutrition, interest in learning specific nutrition topics and desire to complete a clinical nutrition elective. A two-week curriculum covering inpatient and outpatient nutrition care was developed in collaboration with the Center for Human Nutrition.
Results: Forty residents completed the survey. Responders were from all years of training with various career plans after residency. 55% of residents had no prior exposure to clinical nutrition. Only 10% of residents felt they possessed the knowledge to diagnose malnutrition, and only 3% felt confident determining the nutritional needs of their patients. A minority of residents felt comfortable identifying indications for enteral nutrition (30%) and parenteral nutrition (25%), or making nutritional recommendations in a primary care setting (18%). Residents were most interested in learning how to perform a nutrition assessment and determine nutritional requirements (93%), as well as initiate and manage enteral nutrition (93%) and parenteral nutrition (85%). 90% of residents were interested in completing a clinical nutrition elective during their training (Table 1). The two-week nutrition elective was designed to allow didactic training through e-learning modules and hands on training with registered dietitians (RD). Rotations involved working with RDs for education and direct care in the intensive care unit, regular nursing floor, enteral access team, nutrition support team and ambulatory setting. Clear objectives were developed for each nutrition area which included how to identify and diagnose malnutrition, estimate energy and protein needs and how to choose optimal nutritional interventions for patients based on their disease process.
Discussion: Internal medicine residents lack the exposure and knowledge required to address a majority of nutrition related care. Residents are interested in learning various nutrition topics. Implementing a clinical nutrition elective may be effective in addressing this gap in training.
Disclosures:
Michael Delicce, MD, Mary Rath, RD, CNSC, LD, Mattie White, MD, Jason Nasser, MD, Renee Welsh, MS, RD, LD, CNSC, Andrew Ford, MD, Puneet Dhillon, DO, Samia Mazumder, MD, Andrea Jevenn, MEd, RD, LD, CNSC, Donald Kirby, MD, FACG. P4078 - Development of a Clinical Nutrition Elective for an Internal Medicine Residency Program, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Cleveland Clinic, Cleveland, OH
Introduction: A foundational knowledge in nutrition is necessary for internal medicine (IM) residents to identify patients with malnutrition and translate basic nutrition guidelines to improve patient care. However, the majority of medical schools and residency programs do not offer clinical training in nutrition. Therefore, it is imperative that residents have nutrition education incorporated into their training.
Methods: IM residents at our institution were surveyed to assess exposure to nutrition education, baseline knowledge in areas of nutrition, interest in learning specific nutrition topics and desire to complete a clinical nutrition elective. A two-week curriculum covering inpatient and outpatient nutrition care was developed in collaboration with the Center for Human Nutrition.
Results: Forty residents completed the survey. Responders were from all years of training with various career plans after residency. 55% of residents had no prior exposure to clinical nutrition. Only 10% of residents felt they possessed the knowledge to diagnose malnutrition, and only 3% felt confident determining the nutritional needs of their patients. A minority of residents felt comfortable identifying indications for enteral nutrition (30%) and parenteral nutrition (25%), or making nutritional recommendations in a primary care setting (18%). Residents were most interested in learning how to perform a nutrition assessment and determine nutritional requirements (93%), as well as initiate and manage enteral nutrition (93%) and parenteral nutrition (85%). 90% of residents were interested in completing a clinical nutrition elective during their training (Table 1). The two-week nutrition elective was designed to allow didactic training through e-learning modules and hands on training with registered dietitians (RD). Rotations involved working with RDs for education and direct care in the intensive care unit, regular nursing floor, enteral access team, nutrition support team and ambulatory setting. Clear objectives were developed for each nutrition area which included how to identify and diagnose malnutrition, estimate energy and protein needs and how to choose optimal nutritional interventions for patients based on their disease process.
Discussion: Internal medicine residents lack the exposure and knowledge required to address a majority of nutrition related care. Residents are interested in learning various nutrition topics. Implementing a clinical nutrition elective may be effective in addressing this gap in training.
Disclosures:
Michael Delicce indicated no relevant financial relationships.
Mary Rath indicated no relevant financial relationships.
Mattie White indicated no relevant financial relationships.
Jason Nasser indicated no relevant financial relationships.
Renee Welsh indicated no relevant financial relationships.
Andrew Ford indicated no relevant financial relationships.
Puneet Dhillon indicated no relevant financial relationships.
Samia Mazumder indicated no relevant financial relationships.
Andrea Jevenn indicated no relevant financial relationships.
Donald Kirby indicated no relevant financial relationships.
Michael Delicce, MD, Mary Rath, RD, CNSC, LD, Mattie White, MD, Jason Nasser, MD, Renee Welsh, MS, RD, LD, CNSC, Andrew Ford, MD, Puneet Dhillon, DO, Samia Mazumder, MD, Andrea Jevenn, MEd, RD, LD, CNSC, Donald Kirby, MD, FACG. P4078 - Development of a Clinical Nutrition Elective for an Internal Medicine Residency Program, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
