Tuesday Poster Session
Category: Practice Management
P4079 - Building an Iron-Forged Force: A Quality Improvement Project Assessing Diagnostic Outcomes of Iron Deficiency Anemia Among Basic Military Trainees
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- JC
Joseph Cook, MD
San Antonio Uniformed Services Health Education Consortium
Fort Sam Houston, TX
Presenting Author(s)
Joseph Cook, MD1, Geoff Bader, MD2, Charles Miller, MD3
1San Antonio Uniformed Services Health Education Consortium, Fort Sam Houston, TX; 2Brooke Army Medical Center, San Antonio, TX; 3San Antonio Uniformed Services Health Education Consortium, San Antonio, TX
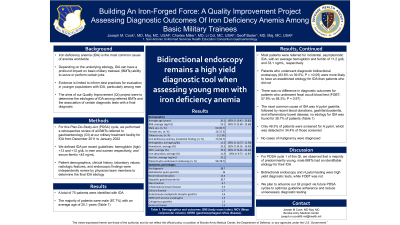
Introduction: Iron deficiency anemia (IDA) is the most common cause of anemia worldwide, with many etiologies leading to significant morbidity and decreased quality of life. Depending on the underlying etiology, IDA can have a profound impact on a basic military trainee's (BMT) ability to serve or perform certain jobs. Evidence is limited to inform best practices for evaluation in younger populations with IDA, particularly among men. The aims of our Quality Improvement (QI) project were to determine the etiologies of IDA among referred BMTs and the association of certain diagnostic tests with a final diagnosis.
Methods: For this Plan-Do-Study-Act (PDSA) cycle, we performed a retrospective review of all BMTs referred to gastroenterology (GI) at our military treatment facility for IDA from December 2011 to January 2022. We defined IDA per recent guidelines: hemoglobin (Hgb) < 13 and < 12 g/dL in men and women, respectively, and serum ferritin < 45 ng/mL. Patient demographics, clinical history, laboratory values, radiologic features, and endoscopic findings were independently reviewed by physician team members to determine the final IDA etiology.
Results: A total of 75 patients were identified with IDA. The majority of patients were male (82.7%) with an average age of 20.1 years (Table 1). Most patients were referred for incidental, asymptomatic IDA, with an average Hgb and ferritin of 11.2 g/dL and 33.1 ng/mL, respectively. Patients who underwent bidirectional endoscopy were more likely to be diagnosed with a specific etiology for IDA than patients who did not (83.8% vs 39.5%; p < 0.05). There was no difference in diagnostic outcomes for patients who underwent fecal occult blood testing (FOBT; 57.9% vs 58.3%; p = 0.97). The most common cause of IDA was H. pylori gastritis, followed by recent blood donations, gastritis/duodenitis, and inflammatory bowel disease; no etiology for IDA was found for 38.7% of patients (Table 1). Only 49.3% of patients were tested for H. pylori, which was detected in 34.4% of those patients who underwent testing. No cases of malignancy were diagnosed.
Discussion: For PDSA Cycle 1 of this QI, we observed that a majority of predominately young, male BMTs had an identifiable etiology for their IDA. Bidirectional endoscopy and H. pylori testing were high yield diagnostic tests, while FOBT was not. We plan to advance our QI project via future PDSA cycles to optimize guideline adherence and reduce unnecessary diagnostic testing.
Disclosures:
Joseph Cook, MD1, Geoff Bader, MD2, Charles Miller, MD3. P4079 - Building an Iron-Forged Force: A Quality Improvement Project Assessing Diagnostic Outcomes of Iron Deficiency Anemia Among Basic Military Trainees, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1San Antonio Uniformed Services Health Education Consortium, Fort Sam Houston, TX; 2Brooke Army Medical Center, San Antonio, TX; 3San Antonio Uniformed Services Health Education Consortium, San Antonio, TX
Introduction: Iron deficiency anemia (IDA) is the most common cause of anemia worldwide, with many etiologies leading to significant morbidity and decreased quality of life. Depending on the underlying etiology, IDA can have a profound impact on a basic military trainee's (BMT) ability to serve or perform certain jobs. Evidence is limited to inform best practices for evaluation in younger populations with IDA, particularly among men. The aims of our Quality Improvement (QI) project were to determine the etiologies of IDA among referred BMTs and the association of certain diagnostic tests with a final diagnosis.
Methods: For this Plan-Do-Study-Act (PDSA) cycle, we performed a retrospective review of all BMTs referred to gastroenterology (GI) at our military treatment facility for IDA from December 2011 to January 2022. We defined IDA per recent guidelines: hemoglobin (Hgb) < 13 and < 12 g/dL in men and women, respectively, and serum ferritin < 45 ng/mL. Patient demographics, clinical history, laboratory values, radiologic features, and endoscopic findings were independently reviewed by physician team members to determine the final IDA etiology.
Results: A total of 75 patients were identified with IDA. The majority of patients were male (82.7%) with an average age of 20.1 years (Table 1). Most patients were referred for incidental, asymptomatic IDA, with an average Hgb and ferritin of 11.2 g/dL and 33.1 ng/mL, respectively. Patients who underwent bidirectional endoscopy were more likely to be diagnosed with a specific etiology for IDA than patients who did not (83.8% vs 39.5%; p < 0.05). There was no difference in diagnostic outcomes for patients who underwent fecal occult blood testing (FOBT; 57.9% vs 58.3%; p = 0.97). The most common cause of IDA was H. pylori gastritis, followed by recent blood donations, gastritis/duodenitis, and inflammatory bowel disease; no etiology for IDA was found for 38.7% of patients (Table 1). Only 49.3% of patients were tested for H. pylori, which was detected in 34.4% of those patients who underwent testing. No cases of malignancy were diagnosed.
Discussion: For PDSA Cycle 1 of this QI, we observed that a majority of predominately young, male BMTs had an identifiable etiology for their IDA. Bidirectional endoscopy and H. pylori testing were high yield diagnostic tests, while FOBT was not. We plan to advance our QI project via future PDSA cycles to optimize guideline adherence and reduce unnecessary diagnostic testing.
Disclosures:
Joseph Cook indicated no relevant financial relationships.
Geoff Bader indicated no relevant financial relationships.
Charles Miller indicated no relevant financial relationships.
Joseph Cook, MD1, Geoff Bader, MD2, Charles Miller, MD3. P4079 - Building an Iron-Forged Force: A Quality Improvement Project Assessing Diagnostic Outcomes of Iron Deficiency Anemia Among Basic Military Trainees, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
