Tuesday Poster Session
Category: Colon
P3083 - Gaining Insight: The Crucial Role of Second-Look Colonoscopy in Managing Massive GI Bleeds From Colonic Arteriovenous Malformation
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MH
Muhammad Hussain, MD
Saint Michael's Medical Center, New York Medical College
Newark, New Jersey
Presenting Author(s)
Muhammad Hussain, MD1, Mohammad Nabil Rayad, MD1, Noreen Mirza, MD1, Theodore DaCosta, DO1, Mohammad Ahmed, MD2, Fnu Marium, MD1, Yatinder Bains, MD1
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2St. George's University, Newark, NJ
Introduction: Gastrointestinal arteriovenous malformations (AVM) are due to thin-walled arteriovenous communications between the mucosa and submucosa of the gastrointestinal wall. These AVMs can vary in size, severity and symptoms. Herein, we report a rare case of hemorrhagic shock due to massive colonic AVM that was diagnosed and managed with a second look colonoscopy.
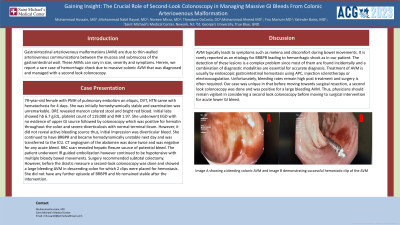
Case Description/Methods: 79-year-old female with PMH of pulmonary embolism on eliquis, DVT, HTN came with hematochezia for 4 days. She was initially hemodynamically stable and examination was unremarkable. DRE revealed maroon colored stool and bright red blood. Initial labs showed hb 6.7 g/dL, platelet count of 119,000 and INR 1.97. She underwent EGD with no evidence of upper GI source followed by colonoscopy which was positive for hematin throughout the colon and severe diverticulosis with normal terminal ileum. However, it did not reveal active bleeding source thus, initial impression was diverticular bleed. She continued to have BRBPR and became hemodynamically unstable next day and was transferred to the ICU. CT angiogram of the abdomen was done twice and was negative for any acute bleed. RBC scan revealed hepatic flexure source of potential bleed. The patient underwent IR guided embolization however continued to be hypotensive with multiple bloody bowel movements. Surgery recommended subtotal colectomy. However, before the drastic measure a second-look colonoscopy was done and showed a large bleeding AVM in descending colon for which 2 clips were placed for hemostasis. She did not have any further episode of BRBPR and hb remained stable after the intervention.
Discussion: AVM typically leads to symptoms such as melena and discomfort during bowel movements. It is rarely reported as an etiology for BRBPR leading to hemorrhagic shock as in our patient. The detection of these lesions is a complex problem since most of them are found incidentally and a combination of diagnostic modalities are essential for accurate diagnosis. Treatment of AVM is usually by endoscopic gastrointestinal hemostasis using APC, injection sclerotherapy or electrocoagulation. Unfortunately, bleeding rates remain high post treatment and surgery is often required. Our case was unique in that before moving towards surgical resection, a second look colonoscopy was done and was positive for a large bleeding AVM. Thus, physicians should remain vigilant in considering a second look colonoscopy before moving to surgical intervention for acute lower GI bleed.

Disclosures:
Muhammad Hussain, MD1, Mohammad Nabil Rayad, MD1, Noreen Mirza, MD1, Theodore DaCosta, DO1, Mohammad Ahmed, MD2, Fnu Marium, MD1, Yatinder Bains, MD1. P3083 - Gaining Insight: The Crucial Role of Second-Look Colonoscopy in Managing Massive GI Bleeds From Colonic Arteriovenous Malformation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2St. George's University, Newark, NJ
Introduction: Gastrointestinal arteriovenous malformations (AVM) are due to thin-walled arteriovenous communications between the mucosa and submucosa of the gastrointestinal wall. These AVMs can vary in size, severity and symptoms. Herein, we report a rare case of hemorrhagic shock due to massive colonic AVM that was diagnosed and managed with a second look colonoscopy.
Case Description/Methods: 79-year-old female with PMH of pulmonary embolism on eliquis, DVT, HTN came with hematochezia for 4 days. She was initially hemodynamically stable and examination was unremarkable. DRE revealed maroon colored stool and bright red blood. Initial labs showed hb 6.7 g/dL, platelet count of 119,000 and INR 1.97. She underwent EGD with no evidence of upper GI source followed by colonoscopy which was positive for hematin throughout the colon and severe diverticulosis with normal terminal ileum. However, it did not reveal active bleeding source thus, initial impression was diverticular bleed. She continued to have BRBPR and became hemodynamically unstable next day and was transferred to the ICU. CT angiogram of the abdomen was done twice and was negative for any acute bleed. RBC scan revealed hepatic flexure source of potential bleed. The patient underwent IR guided embolization however continued to be hypotensive with multiple bloody bowel movements. Surgery recommended subtotal colectomy. However, before the drastic measure a second-look colonoscopy was done and showed a large bleeding AVM in descending colon for which 2 clips were placed for hemostasis. She did not have any further episode of BRBPR and hb remained stable after the intervention.
Discussion: AVM typically leads to symptoms such as melena and discomfort during bowel movements. It is rarely reported as an etiology for BRBPR leading to hemorrhagic shock as in our patient. The detection of these lesions is a complex problem since most of them are found incidentally and a combination of diagnostic modalities are essential for accurate diagnosis. Treatment of AVM is usually by endoscopic gastrointestinal hemostasis using APC, injection sclerotherapy or electrocoagulation. Unfortunately, bleeding rates remain high post treatment and surgery is often required. Our case was unique in that before moving towards surgical resection, a second look colonoscopy was done and was positive for a large bleeding AVM. Thus, physicians should remain vigilant in considering a second look colonoscopy before moving to surgical intervention for acute lower GI bleed.

Figure: Image A showing a bleeding colonic AVM and Image B demonstrating successful hemostatic clip of the AVM
Disclosures:
Muhammad Hussain indicated no relevant financial relationships.
Mohammad Nabil Rayad indicated no relevant financial relationships.
Noreen Mirza indicated no relevant financial relationships.
Theodore DaCosta indicated no relevant financial relationships.
Mohammad Ahmed indicated no relevant financial relationships.
Fnu Marium indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Muhammad Hussain, MD1, Mohammad Nabil Rayad, MD1, Noreen Mirza, MD1, Theodore DaCosta, DO1, Mohammad Ahmed, MD2, Fnu Marium, MD1, Yatinder Bains, MD1. P3083 - Gaining Insight: The Crucial Role of Second-Look Colonoscopy in Managing Massive GI Bleeds From Colonic Arteriovenous Malformation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
