Tuesday Poster Session
Category: Practice Management
P4087 - Fecal Occult Testing for Hospitalized Patients… Is This Still a Thing?
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MB
Mohammad Bilal, MD
Rochester General Hospital
Rochester, New York
Presenting Author(s)
Mohammad Bilal, MD1, Ese Uwagbale, MD1, Le Yu Naing, MD2, Faizan Khalid, MD3, Basil Verghese, MD1
1Rochester General Hospital, Rochester, NY; 2University of Louisville, Louisville, KY; 3Emory University, Atlanta, GA
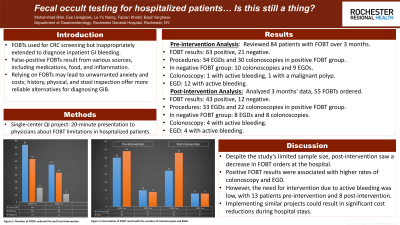
Introduction: While FOBTs are valuable as screening tests for CRC in the outpatient setting, their use has been extended to diagnose GI bleeding in the inpatient setting without supporting data. False-positive FOBT results can occur from ingested blood from epistaxis, hemoptysis, gingival bleeding, inflammation (esophagitis, gastritis, IBD), insignificant blood loss induced by medications (aspirin, NSAIDs), alcohol, ingestion of food (meats, broccoli, cauliflower). Incorrect test results may lead to unnecessary anxiety and increased cost from preventable hospital stay and further testing. Alternatively a careful history, physical examination or visual inspection of the stool are more reliable to establish GIB as etiology of anemia.
Methods: We conducted a single-center QI project which involved a 20-minute presentation for physicians highlighting the limitations of performing FOBT on hospitalized patients.
Results: Pre-intervention analysis included 3 months’ review of hospitalized patients who had FOBT done. Total sample size was 84 patients. FOBT was positive in 63 patients and negative in 21. Of the 63 patients with a positive FOBT, 34 underwent EGD and 30 underwent colonoscopy. Of 21 patients with negative FOBT, 10 had colonoscopy and 9 had EGD. Of the 40 patients who underwent colonoscopy 1 had active bleeding requiring intervention and 1 was found to have a malignant polyp. Of 43 patients who had EGD, 12 had active bleeding requiring intervention.
Post-intervention, 3 months’ data analysis revealed that total number of FOBT ordered on hospitalized patients decreased to 55. FOBT was positive in 43 patients and negative in 12 patients. 33 out of 43 patients with positive FOBT underwent EGD and 22 underwent colonoscopy. 8 out of 12 patients with negative FOBT had EGD and 8 had a colonoscopy. Of 30 patients who had colonoscopy, 4 had active bleeding requiring intervention and of the 41 patients who had EGD, 4 had active bleeding requiring intervention.
Discussion: Although our study did not have a sufficient sample size to achieve statistical significance, the number of FOBTs ordered in our hospital decreased in the post-intervention group. Positive FOBT results correlated with higher rates of colonoscopy and EGD. However, only 13 patients pre-intervention and 8 patients post-intervention had active bleeding necessitating intervention. Implementing similar projects can lead to significant cost reductions in hospital stays.

Disclosures:
Mohammad Bilal, MD1, Ese Uwagbale, MD1, Le Yu Naing, MD2, Faizan Khalid, MD3, Basil Verghese, MD1. P4087 - Fecal Occult Testing for Hospitalized Patients… Is This Still a Thing?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2University of Louisville, Louisville, KY; 3Emory University, Atlanta, GA
Introduction: While FOBTs are valuable as screening tests for CRC in the outpatient setting, their use has been extended to diagnose GI bleeding in the inpatient setting without supporting data. False-positive FOBT results can occur from ingested blood from epistaxis, hemoptysis, gingival bleeding, inflammation (esophagitis, gastritis, IBD), insignificant blood loss induced by medications (aspirin, NSAIDs), alcohol, ingestion of food (meats, broccoli, cauliflower). Incorrect test results may lead to unnecessary anxiety and increased cost from preventable hospital stay and further testing. Alternatively a careful history, physical examination or visual inspection of the stool are more reliable to establish GIB as etiology of anemia.
Methods: We conducted a single-center QI project which involved a 20-minute presentation for physicians highlighting the limitations of performing FOBT on hospitalized patients.
Results: Pre-intervention analysis included 3 months’ review of hospitalized patients who had FOBT done. Total sample size was 84 patients. FOBT was positive in 63 patients and negative in 21. Of the 63 patients with a positive FOBT, 34 underwent EGD and 30 underwent colonoscopy. Of 21 patients with negative FOBT, 10 had colonoscopy and 9 had EGD. Of the 40 patients who underwent colonoscopy 1 had active bleeding requiring intervention and 1 was found to have a malignant polyp. Of 43 patients who had EGD, 12 had active bleeding requiring intervention.
Post-intervention, 3 months’ data analysis revealed that total number of FOBT ordered on hospitalized patients decreased to 55. FOBT was positive in 43 patients and negative in 12 patients. 33 out of 43 patients with positive FOBT underwent EGD and 22 underwent colonoscopy. 8 out of 12 patients with negative FOBT had EGD and 8 had a colonoscopy. Of 30 patients who had colonoscopy, 4 had active bleeding requiring intervention and of the 41 patients who had EGD, 4 had active bleeding requiring intervention.
Discussion: Although our study did not have a sufficient sample size to achieve statistical significance, the number of FOBTs ordered in our hospital decreased in the post-intervention group. Positive FOBT results correlated with higher rates of colonoscopy and EGD. However, only 13 patients pre-intervention and 8 patients post-intervention had active bleeding necessitating intervention. Implementing similar projects can lead to significant cost reductions in hospital stays.

Figure: Fig 1: Number of FOBTs ordered pre and post intervention
Fig 2: Association of FOBT results with the number of Colonoscopies & EGDs
Fig 2: Association of FOBT results with the number of Colonoscopies & EGDs
Disclosures:
Mohammad Bilal indicated no relevant financial relationships.
Ese Uwagbale indicated no relevant financial relationships.
Le Yu Naing indicated no relevant financial relationships.
Faizan Khalid indicated no relevant financial relationships.
Basil Verghese indicated no relevant financial relationships.
Mohammad Bilal, MD1, Ese Uwagbale, MD1, Le Yu Naing, MD2, Faizan Khalid, MD3, Basil Verghese, MD1. P4087 - Fecal Occult Testing for Hospitalized Patients… Is This Still a Thing?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
