Tuesday Poster Session
Category: Practice Management
P4089 - Effectiveness of a Structured Education Intervention in Improving GERD Symptom Reassessment and Reducing Long-term PPI Use in an Underserved Population
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Leen Hasan, MD
UCONN Health
New York , NY
Presenting Author(s)
Award: Presidential Poster Award
Leen Hasan, MD1, Simon Abi Saleh, MD1, Ruchir Paladiya, MBBS1, Amanda Frondella, MD1, Cunegundo Vergara, MD2, Joel Wilken, DO2
1UCONN Health, Farmington, CT; 2Hartford Hospital, Hartford, CT
Introduction: This study aims to evaluate a structured education intervention in adult primary care (APC) for managing Gastroesophageal Reflux Disease (GERD) and reducing unnecessary long-term Proton Pump Inhibitors (PPIs) use in an underserved population.
Methods: The structured education intervention spanned from June 2022 - May 2023 and involved weekly lectures delivered over 1 month to primary care providers. The lectures emphasized the importance of GERD symptom reasessment, lifestyle changes, GI referrals, and appropriate PPI use. We implemented a smart phrase in our EMR to document symptom reassessment. Using the APC clinic database, we reviewed adults (≥18 years old) prescribed PPI therapy for GERD over a 2-year period (pre- and post-intervention). We compared the proportion of patients who underwent GERD symptom reassessment after 8 weeks of PPI initiation before and after the intervention using McNemar's test for binary matched-pairs data.
Results: Out of the 132 patients included in the study, 75% were Hispanic, 10% African American and 10% Caucasian. Prior to the intervention, only 38 patients (29%) underwent proper symptom assessment after 8 weeks of initiating PPI therapy. Among these patients, 37 (97%) continued the same PPI dose, 9 (24%) were referred to GI specialists, 3 (8%) were recommended lifestyle modifications, and 1 patient (3%) had their PPI discontinued. Following the intervention, 6 patients were lost to follow-up; among the remaining 126 patients, GERD symptoms were assessed in 62 (47%) individuals. Out of the assessed patients, 50 (81%) remained on the same PPI dose, 25 (40%) were referred to GI specialists, 14 (23%) were advised on lifestyle modifications, and 12 (19%) had their PPI dose reduced or discontinued. Using McNemar's test, the education intervention demonstrated a statistically significant 25% increase in GERD symptom reassessment (P < 0.0001).
Discussion: In this underserved population, we identified a notable prevalence of inappropriate long-term PPI use for treating GERD which may be attributed to their perceived safe profile and lack of awareness of potential side effects. Our intervention had a significant impact on the reassessment of GERD symptoms, leading to subsequent changes in management. Timely evaluation of GERD symptoms following an 8-week trial of PPI therapy is crucial, as a lack of response may necessitate referral to the GI clinic. Moreover, avoiding prolonged, unnecessary PPI therapy is important due to the associated adverse events.

Disclosures:
Leen Hasan, MD1, Simon Abi Saleh, MD1, Ruchir Paladiya, MBBS1, Amanda Frondella, MD1, Cunegundo Vergara, MD2, Joel Wilken, DO2. P4089 - Effectiveness of a Structured Education Intervention in Improving GERD Symptom Reassessment and Reducing Long-term PPI Use in an Underserved Population, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Leen Hasan, MD1, Simon Abi Saleh, MD1, Ruchir Paladiya, MBBS1, Amanda Frondella, MD1, Cunegundo Vergara, MD2, Joel Wilken, DO2
1UCONN Health, Farmington, CT; 2Hartford Hospital, Hartford, CT
Introduction: This study aims to evaluate a structured education intervention in adult primary care (APC) for managing Gastroesophageal Reflux Disease (GERD) and reducing unnecessary long-term Proton Pump Inhibitors (PPIs) use in an underserved population.
Methods: The structured education intervention spanned from June 2022 - May 2023 and involved weekly lectures delivered over 1 month to primary care providers. The lectures emphasized the importance of GERD symptom reasessment, lifestyle changes, GI referrals, and appropriate PPI use. We implemented a smart phrase in our EMR to document symptom reassessment. Using the APC clinic database, we reviewed adults (≥18 years old) prescribed PPI therapy for GERD over a 2-year period (pre- and post-intervention). We compared the proportion of patients who underwent GERD symptom reassessment after 8 weeks of PPI initiation before and after the intervention using McNemar's test for binary matched-pairs data.
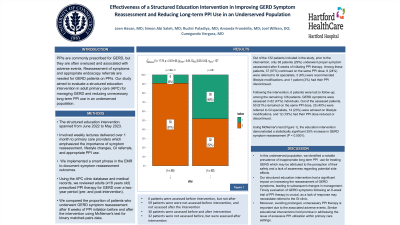
Results: Out of the 132 patients included in the study, 75% were Hispanic, 10% African American and 10% Caucasian. Prior to the intervention, only 38 patients (29%) underwent proper symptom assessment after 8 weeks of initiating PPI therapy. Among these patients, 37 (97%) continued the same PPI dose, 9 (24%) were referred to GI specialists, 3 (8%) were recommended lifestyle modifications, and 1 patient (3%) had their PPI discontinued. Following the intervention, 6 patients were lost to follow-up; among the remaining 126 patients, GERD symptoms were assessed in 62 (47%) individuals. Out of the assessed patients, 50 (81%) remained on the same PPI dose, 25 (40%) were referred to GI specialists, 14 (23%) were advised on lifestyle modifications, and 12 (19%) had their PPI dose reduced or discontinued. Using McNemar's test, the education intervention demonstrated a statistically significant 25% increase in GERD symptom reassessment (P < 0.0001).
Discussion: In this underserved population, we identified a notable prevalence of inappropriate long-term PPI use for treating GERD which may be attributed to their perceived safe profile and lack of awareness of potential side effects. Our intervention had a significant impact on the reassessment of GERD symptoms, leading to subsequent changes in management. Timely evaluation of GERD symptoms following an 8-week trial of PPI therapy is crucial, as a lack of response may necessitate referral to the GI clinic. Moreover, avoiding prolonged, unnecessary PPI therapy is important due to the associated adverse events.

Figure: McNemar's test demonstrating a 25% increase in GERD symptom reassessment (P < 0.0001)
0: GERD symptoms not reassessed, 1: GERD symptoms reassessed
0: GERD symptoms not reassessed, 1: GERD symptoms reassessed
Disclosures:
Leen Hasan indicated no relevant financial relationships.
Simon Abi Saleh indicated no relevant financial relationships.
Ruchir Paladiya indicated no relevant financial relationships.
Amanda Frondella indicated no relevant financial relationships.
Cunegundo Vergara indicated no relevant financial relationships.
Joel Wilken indicated no relevant financial relationships.
Leen Hasan, MD1, Simon Abi Saleh, MD1, Ruchir Paladiya, MBBS1, Amanda Frondella, MD1, Cunegundo Vergara, MD2, Joel Wilken, DO2. P4089 - Effectiveness of a Structured Education Intervention in Improving GERD Symptom Reassessment and Reducing Long-term PPI Use in an Underserved Population, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


