Tuesday Poster Session
Category: Colon
P3091 - A Myco-Misadventure
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Keerthi Thallapureddy, MD
UT Health San Antonio
San Antonio, TX
Presenting Author(s)
Keerthi Thallapureddy, MD1, Grace Hopp, DO, MBA1, Sarah Hackman, MD1, Lisa Pedicone, PhD2, Carmen Landaverde, MD3, Fabian Rodas, MD3, Jan Petrasek, MD, PhD3, Fred Poordad, MD3, Eric Lawitz, MD3, Eugenia Tsai, MD3
1UT Health San Antonio, San Antonio, TX; 2Texas Liver Institute, San Antonio, TX; 3UT Health San Antonio, Texas Liver Institute, San Antonio, TX
Introduction: Mycophenolate mofetil (MMF)-induced colitis is a well-recognized etiology of diarrhea in solid organ transplant (SOT) recipients. The latency period between initiation of the drug and onset of symptoms is 6 months to 15 years. We present an unusual case of MMF-induced colitis in a liver transplant recipient a month after initiation of the drug.
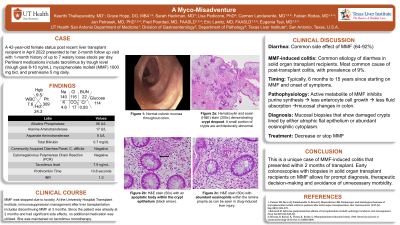
Case Description/Methods: A 42 year-old female liver transplant recipient for alcohol-related cirrhosis presents at her two-month visit and reports up to seven episodes of watery loose stools per day for the past month. A community acquired diarrhea panel was negative for infectious etiology and MMF dose was decreased from 750mg twice daily to 500mg twice daily. Laboratory results and graft function remained stable throughout this time. A colonoscopy showed normal-appearing colonic mucosa. Random colonic biopsies revealed crypt dropout (Figure 1a), with eosinophilic crypt abscesses and crypt cell apoptosis (Figure 1b) and increased eosinophils (Figure 1c), consistent with MMF-induced colitis. MMF dose was stopped earlier than per institution protocol with resolution of symptoms.
Discussion: MMF is often a lifelong mainstay of immunosuppressive regimens in SOT recipients. Early discontinuation can lead to risk of organ rejection. One of the most common side effects is diarrhea (64-92%). However, only 2-9% of those with diarrhea have MMF-colitis. Mycophenolic acid, the active metabolite of MMF, inhibits monophosphate dehydrogenase, an enzyme essential to purine synthesis. Enterocytes depend on purine synthesis for bowel epithelial cell growth with proliferation of both T and B-cells. Disruption of this process leads to less fluid absorption and mucosal changes in the colon, typically ulcerations. Diagnosis is made by mucosal biopsies, which will demonstrate damaged crypts lined by either atrophic-flattened epithelium or, as seen in this case, cells with abundant eosinophilic cytoplasm. Treatment is decreasing or discontinuing MMF.
This case is atypical due to the rapid onset of symptoms and endoscopically healthy appearing colonic mucosa. Early colonoscopy with biopsies in SOT recipients on MMF allows for prompt diagnosis, therapeutic decision-making and avoiding unnecessary morbidity.

Disclosures:
Keerthi Thallapureddy, MD1, Grace Hopp, DO, MBA1, Sarah Hackman, MD1, Lisa Pedicone, PhD2, Carmen Landaverde, MD3, Fabian Rodas, MD3, Jan Petrasek, MD, PhD3, Fred Poordad, MD3, Eric Lawitz, MD3, Eugenia Tsai, MD3. P3091 - A Myco-Misadventure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UT Health San Antonio, San Antonio, TX; 2Texas Liver Institute, San Antonio, TX; 3UT Health San Antonio, Texas Liver Institute, San Antonio, TX
Introduction: Mycophenolate mofetil (MMF)-induced colitis is a well-recognized etiology of diarrhea in solid organ transplant (SOT) recipients. The latency period between initiation of the drug and onset of symptoms is 6 months to 15 years. We present an unusual case of MMF-induced colitis in a liver transplant recipient a month after initiation of the drug.
Case Description/Methods: A 42 year-old female liver transplant recipient for alcohol-related cirrhosis presents at her two-month visit and reports up to seven episodes of watery loose stools per day for the past month. A community acquired diarrhea panel was negative for infectious etiology and MMF dose was decreased from 750mg twice daily to 500mg twice daily. Laboratory results and graft function remained stable throughout this time. A colonoscopy showed normal-appearing colonic mucosa. Random colonic biopsies revealed crypt dropout (Figure 1a), with eosinophilic crypt abscesses and crypt cell apoptosis (Figure 1b) and increased eosinophils (Figure 1c), consistent with MMF-induced colitis. MMF dose was stopped earlier than per institution protocol with resolution of symptoms.
Discussion: MMF is often a lifelong mainstay of immunosuppressive regimens in SOT recipients. Early discontinuation can lead to risk of organ rejection. One of the most common side effects is diarrhea (64-92%). However, only 2-9% of those with diarrhea have MMF-colitis. Mycophenolic acid, the active metabolite of MMF, inhibits monophosphate dehydrogenase, an enzyme essential to purine synthesis. Enterocytes depend on purine synthesis for bowel epithelial cell growth with proliferation of both T and B-cells. Disruption of this process leads to less fluid absorption and mucosal changes in the colon, typically ulcerations. Diagnosis is made by mucosal biopsies, which will demonstrate damaged crypts lined by either atrophic-flattened epithelium or, as seen in this case, cells with abundant eosinophilic cytoplasm. Treatment is decreasing or discontinuing MMF.
This case is atypical due to the rapid onset of symptoms and endoscopically healthy appearing colonic mucosa. Early colonoscopy with biopsies in SOT recipients on MMF allows for prompt diagnosis, therapeutic decision-making and avoiding unnecessary morbidity.

Figure: Figure 1 (a-c) Histological findings on colon biopsy consistent with mycophenolate mofetil-induced colitis. (a) Hematoxylin and eosin (H&E) stain (200x) demonstrating crypt dropout. Remaining crypts are architecturally abnormal (*); (b) H&E stain (50x) with an apoptotic body within the crypt epithelium (black arrow); (c) H&E stain (50x) with abundant eosinophils within the lamina propria as can be seen in drug-induced liver injury
Disclosures:
Keerthi Thallapureddy indicated no relevant financial relationships.
Grace Hopp indicated no relevant financial relationships.
Sarah Hackman indicated no relevant financial relationships.
Lisa Pedicone indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Eric Lawitz: 89Bio, Inc – Grant/Research Support. AbbVie – Grant/Research Support, Speakers Bureau. Akero – Advisor or Review Panel Member, Grant/Research Support. Allergan – Grant/Research Support. Alnylam – Grant/Research Support. Amgen – Grant/Research Support. Ascelia Pharma – Grant/Research Support. AstraZeneca – Grant/Research Support. Axcella Health – Grant/Research Support. Boehringer Ingelheim – Advisor or Review Panel Member, Grant/Research Support. Bristol Myers Squibb – Advisor or Review Panel Member, Grant/Research Support. Conatus Pharmaceuticals – Grant/Research Support. Cymabay – Grant/Research Support. CytoDyn – Grant/Research Support. DSM – Grant/Research Support. Durect Corporation – Grant/Research Support. Gilead – Speakers Bureau. Intercept – Advisor or Review Panel Member, Grant/Research Support, Speakers Bureau. Metacrine – Advisor or Review Panel Member. Novo Nordisk – Advisor or Review Panel Member. Sagimet – Advisor or Review Panel Member. Terns – Advisor or Review Panel Member.
Eugenia Tsai indicated no relevant financial relationships.
Keerthi Thallapureddy, MD1, Grace Hopp, DO, MBA1, Sarah Hackman, MD1, Lisa Pedicone, PhD2, Carmen Landaverde, MD3, Fabian Rodas, MD3, Jan Petrasek, MD, PhD3, Fred Poordad, MD3, Eric Lawitz, MD3, Eugenia Tsai, MD3. P3091 - A Myco-Misadventure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
