Tuesday Poster Session
Category: Practice Management
P4094 - Proton Pump Inhibitor Over-Utilization in Patients Discharged from Intensive Care Units: A Retrospective Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Peter Bhandari, MD
Lenox Hill Hospital, Northwell Health
New York, NY
Presenting Author(s)
Peter Bhandari, MD1, Varsha Sridhar, DO2, Samantha Rubin, DO1, Samip Shah, MD2, Aditya Sreenivasan, MD3, Ethan Fried, MD1
1Lenox Hill Hospital, Northwell Health, New York, NY; 2Lenox Hill Hospital, New York, NY; 3Northwell Health, New York, NY
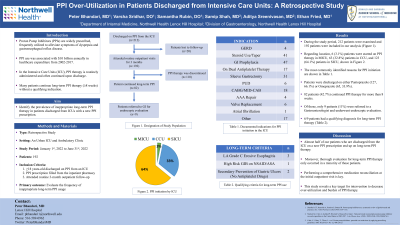
Introduction: Proton Pump Inhibitors (PPIs) </span><span xml:lang="EN-US" data-contrast="none">are one of the most widely prescribed medications, frequently utilized to alleviate symptoms of dyspepsia and gastroesophageal reflux disease. In the Intensive Care Unit (ICU) setting, PPI therapy is routinely administered prophylactically and often continued upon discharge. Many of these patients present to ambulatory clinics without a qualifying indication for continued PPI therapy. This study aims to identify the prevalence of inappropriate long-term PPI therapy in patients discharged from our ICUs with a new PPI prescription.
Methods: We performed a retrospective chart review from January 2022 to June 2022 on ICU patients who were initiated and discharged on PPI therapy using our inpatient pharmacy. Patients were subsequently followed as an outpatient for 3 months to identify individuals who were continued on long-term ( > 8 weeks) PPI therapy. Inclusion criteria of our study involved individuals ≥18 years-old who were prescribed and discharged on PPI therapy from an ICU setting. The primary outcome for the study was the number of inappropriate long-term PPI usage.
Results: During this study period, 212 patients were discharged from the ICU on PPI therapy. Of these, 20 (9.4%) were lost to follow up. The remaining 192 patients were included in our analysis. Of the 192, 97 (50.5%) were male. Regarding race distribution, White 82 (42.7%), African American 30 (15.6%), Asian 14 (7.3%), and Other 66 (34.4%). Regarding location, 6 (3.1%) patients were started on PPI therapy in Medical Intensive Care Units (MICU), 63 (32.8%) patients in Cardiac Care Units (CCU), and 123 (64.1%) patients in Surgical Intensive Care Units (SICU). The most commonly identified reasons for PPI initiation are shown in Table 1. Patients were discharged on either Pantoprazole (127, 66.1%) or Omeprazole (65, 33.9%). On subsequent outpatient visits, 82 (42.7%) patients were continued on PPI therapy for more than 8 weeks. Of these, 9 (11%) patients were referred to a Gastroenterologist and underwent endoscopic evaluation. Of those who underwent endoscopic evaluation, 6 patients had a qualifying diagnosis for long-term PPI therapy.
Discussion: Our findings suggest that almost half of our patients who are discharged from the ICU on a new PPI prescription end up on long-term PPI therapy. Moreover, thorough evaluation for long-term PPI therapy only occurred in a minority of these patients. This study reveals a key target for intervention to decrease over-utilization and burden of PPI therapy.
Disclosures:
Peter Bhandari, MD1, Varsha Sridhar, DO2, Samantha Rubin, DO1, Samip Shah, MD2, Aditya Sreenivasan, MD3, Ethan Fried, MD1. P4094 - Proton Pump Inhibitor Over-Utilization in Patients Discharged from Intensive Care Units: A Retrospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Lenox Hill Hospital, Northwell Health, New York, NY; 2Lenox Hill Hospital, New York, NY; 3Northwell Health, New York, NY
Introduction: Proton Pump Inhibitors (PPIs) </span><span xml:lang="EN-US" data-contrast="none">are one of the most widely prescribed medications, frequently utilized to alleviate symptoms of dyspepsia and gastroesophageal reflux disease. In the Intensive Care Unit (ICU) setting, PPI therapy is routinely administered prophylactically and often continued upon discharge. Many of these patients present to ambulatory clinics without a qualifying indication for continued PPI therapy. This study aims to identify the prevalence of inappropriate long-term PPI therapy in patients discharged from our ICUs with a new PPI prescription.
Methods: We performed a retrospective chart review from January 2022 to June 2022 on ICU patients who were initiated and discharged on PPI therapy using our inpatient pharmacy. Patients were subsequently followed as an outpatient for 3 months to identify individuals who were continued on long-term ( > 8 weeks) PPI therapy. Inclusion criteria of our study involved individuals ≥18 years-old who were prescribed and discharged on PPI therapy from an ICU setting. The primary outcome for the study was the number of inappropriate long-term PPI usage.
Results: During this study period, 212 patients were discharged from the ICU on PPI therapy. Of these, 20 (9.4%) were lost to follow up. The remaining 192 patients were included in our analysis. Of the 192, 97 (50.5%) were male. Regarding race distribution, White 82 (42.7%), African American 30 (15.6%), Asian 14 (7.3%), and Other 66 (34.4%). Regarding location, 6 (3.1%) patients were started on PPI therapy in Medical Intensive Care Units (MICU), 63 (32.8%) patients in Cardiac Care Units (CCU), and 123 (64.1%) patients in Surgical Intensive Care Units (SICU). The most commonly identified reasons for PPI initiation are shown in Table 1. Patients were discharged on either Pantoprazole (127, 66.1%) or Omeprazole (65, 33.9%). On subsequent outpatient visits, 82 (42.7%) patients were continued on PPI therapy for more than 8 weeks. Of these, 9 (11%) patients were referred to a Gastroenterologist and underwent endoscopic evaluation. Of those who underwent endoscopic evaluation, 6 patients had a qualifying diagnosis for long-term PPI therapy.
Discussion: Our findings suggest that almost half of our patients who are discharged from the ICU on a new PPI prescription end up on long-term PPI therapy. Moreover, thorough evaluation for long-term PPI therapy only occurred in a minority of these patients. This study reveals a key target for intervention to decrease over-utilization and burden of PPI therapy.
Disclosures:
Peter Bhandari indicated no relevant financial relationships.
Varsha Sridhar indicated no relevant financial relationships.
Samantha Rubin indicated no relevant financial relationships.
Samip Shah indicated no relevant financial relationships.
Aditya Sreenivasan indicated no relevant financial relationships.
Ethan Fried indicated no relevant financial relationships.
Peter Bhandari, MD1, Varsha Sridhar, DO2, Samantha Rubin, DO1, Samip Shah, MD2, Aditya Sreenivasan, MD3, Ethan Fried, MD1. P4094 - Proton Pump Inhibitor Over-Utilization in Patients Discharged from Intensive Care Units: A Retrospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
