Tuesday Poster Session
Category: Colon
P3094 - Ulcerating Amebic Colitis in an Asymptomatic, Immunocompetent Patient
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Jackson E. Rudolph, BS
Uniformed Services University of the Health Sciences
Joint Base Lewis-McChord, WA
Presenting Author(s)
Jackson E. Rudolph, BS1, Brittney Graham, DO2, Andrew Mertz, MD3, Ryan Kwok, MD2
1Uniformed Services University of the Health Sciences, Joint Base Lewis-McChord, WA; 2Madigan Army Medical Center, Joint Base Lewis-McChord, WA; 3Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Amebic colitis is most commonly caused by the parasite Entamoeba histolytica, which infiltrates colonic mucosa and often causes abdominal pain, diarrhea, and hematochezia. Infection with E. histolytica usually results from fecal-oral transmission due to contaminated drinking water. Infections are uncommon in the United States except among immigrants and travelers from endemic regions. Furthermore, progression to amebic colitis is unusual in immunocompetent patients. We present the case of an asymptomatic active duty service member (ADSM) diagnosed with ulcerating amebic colitis after presenting with a positive fecal immunohistochemical test (FIT).
Case Description/Methods: A 42-year-old male ADSM presented for further evaluation of a positive FIT obtained for military readiness. He endorsed normal, formed bowel movements and denied any associated symptoms to include abdominal pain, diarrhea, or bloody stools.
The patient was previously stationed in Korea from 2018-2019. He reported travel to Thailand in March 2019 where he ate local fare and used tap water. He did not recall any gastrointestinal symptoms during these periods. Physical exam and initial labs were unremarkable.
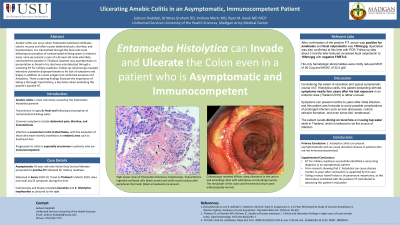
Colonoscopy revealed diffuse, deep ulceration in the cecum and ascending colon with edematous surrounding mucosa. The remainder of the colon and the terminal ileum were endoscopically normal. Biopsies of the ulcers demonstrated numerous trophozoites concerning for amebic colitis with stool antigen testing confirming presence of E. histolytica.
The patient was treated with metronidazole for 14 days and paromomycin for 7 days and remained asymptomatic in follow-up.
Discussion: While most E. histolytica infections are asymptomatic, progression to amebic colitis with ulceration is typically associated with diarrhea and hematochezia. Disease may occur months to years after initial infection and rarely can present with hepatic abscess formation in later stages of disease. Endoscopic findings in amebic colitis vary from discrete colonic ulcers, which was seen in our case, to diffuse ulceration, stricturing, and even with tumor-like “amebomas”. Amebae are typically found in the periphery of the lesions suggesting that biopsies from this area may be of highest yield. Our case demonstrates the importance of obtaining a robust travel history in any patient presenting with concerns for infectious colitis, as even remote exposure may lead to present infection.

Disclosures:
Jackson E. Rudolph, BS1, Brittney Graham, DO2, Andrew Mertz, MD3, Ryan Kwok, MD2. P3094 - Ulcerating Amebic Colitis in an Asymptomatic, Immunocompetent Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Uniformed Services University of the Health Sciences, Joint Base Lewis-McChord, WA; 2Madigan Army Medical Center, Joint Base Lewis-McChord, WA; 3Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Amebic colitis is most commonly caused by the parasite Entamoeba histolytica, which infiltrates colonic mucosa and often causes abdominal pain, diarrhea, and hematochezia. Infection with E. histolytica usually results from fecal-oral transmission due to contaminated drinking water. Infections are uncommon in the United States except among immigrants and travelers from endemic regions. Furthermore, progression to amebic colitis is unusual in immunocompetent patients. We present the case of an asymptomatic active duty service member (ADSM) diagnosed with ulcerating amebic colitis after presenting with a positive fecal immunohistochemical test (FIT).
Case Description/Methods: A 42-year-old male ADSM presented for further evaluation of a positive FIT obtained for military readiness. He endorsed normal, formed bowel movements and denied any associated symptoms to include abdominal pain, diarrhea, or bloody stools.
The patient was previously stationed in Korea from 2018-2019. He reported travel to Thailand in March 2019 where he ate local fare and used tap water. He did not recall any gastrointestinal symptoms during these periods. Physical exam and initial labs were unremarkable.
Colonoscopy revealed diffuse, deep ulceration in the cecum and ascending colon with edematous surrounding mucosa. The remainder of the colon and the terminal ileum were endoscopically normal. Biopsies of the ulcers demonstrated numerous trophozoites concerning for amebic colitis with stool antigen testing confirming presence of E. histolytica.
The patient was treated with metronidazole for 14 days and paromomycin for 7 days and remained asymptomatic in follow-up.
Discussion: While most E. histolytica infections are asymptomatic, progression to amebic colitis with ulceration is typically associated with diarrhea and hematochezia. Disease may occur months to years after initial infection and rarely can present with hepatic abscess formation in later stages of disease. Endoscopic findings in amebic colitis vary from discrete colonic ulcers, which was seen in our case, to diffuse ulceration, stricturing, and even with tumor-like “amebomas”. Amebae are typically found in the periphery of the lesions suggesting that biopsies from this area may be of highest yield. Our case demonstrates the importance of obtaining a robust travel history in any patient presenting with concerns for infectious colitis, as even remote exposure may lead to present infection.

Figure: Figure 1. High power view of Entamoeba histolytica trophozoites. Characteristic ingested red blood cells (black arrow) and small round nucleus with peripheral chromatin (black arrowhead) are present. Hematoxylin-eosin, Oil immersion 50X objective. Colonoscopy image in the inset illustrates extensive ulceration.
Disclosures:
Jackson Rudolph indicated no relevant financial relationships.
Brittney Graham indicated no relevant financial relationships.
Andrew Mertz indicated no relevant financial relationships.
Ryan Kwok indicated no relevant financial relationships.
Jackson E. Rudolph, BS1, Brittney Graham, DO2, Andrew Mertz, MD3, Ryan Kwok, MD2. P3094 - Ulcerating Amebic Colitis in an Asymptomatic, Immunocompetent Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
