Tuesday Poster Session
Category: Small Intestine
P4105 - Impact of Malnutrition in Patients Hospitalized With Celiac Disease: Analysis of National Inpatient Sample 2016-2020
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Shivam Kalra, MBBS
Trident Medical Center
North Charleston, SC
Presenting Author(s)
Kanwal Bains, MBBS, CNSC1, Aalam Sohal, MD2, Hunza Chaudhry, MD3, Ishandeep Singh, MBBS4, Shivam Kalra, MBBS5, Dino Dukovic, BS6, Avin Aggarwal, MBBS7
1University of Arizona, Tucson, AZ; 2Liver Institute Northwest, Seattle, WA; 3University of California San Francisco, Fresno, CA; 4Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 5Trident Medical Center, Charleston, SC; 6Ross University School of Medicine, Maramar, FL; 7University of Arizona College of Medicine, Tucson, AZ
Introduction: Celiac disease (CD) is a T cell-mediated gluten sensitivity that results in villous atrophy in the small intestine leading to chronic malabsorption. Although malnutrition is a known complication in patients with CD, its impact on outcomes is unknown. We assessed the impact of malnutrition on in-hospital outcomes in patients with CD.
Methods: National Inpatient Sample 2016-2020 was used to identify adult patients with a primary discharge diagnosis of CD. Patients with missing demographics or mortality were excluded from the analysis. Data were collected on patient demographics, hospital characteristics, Charlson Comorbidity Index (CCI), and Charlson comorbidities. We compared the incidence of outcomes, including mortality, deep vein thrombosis (DVT), sepsis, acute kidney injury (AKI), intensive care unit(ICU) admission, length of stay (LOS), and total hospitalization charges (THC) between the two groups. The relationship between mortality, LOS, and total hospitalization charges was analyzed using the multivariate regression model.
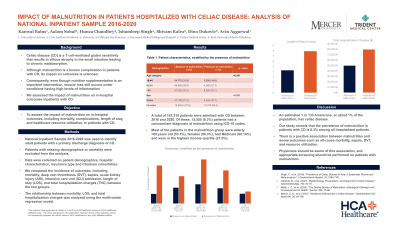
Results: A total of 187,310 patients with CD were included in the analysis. Of these, 15,555 (8.3%) patients were malnourished. The majority of the patients in the malnourished group were elderly > 65 yrs age (53.1%), female (66.3%), had Medicare (60.14%), and were in the highest income quartile (27.9%). The incidence of in-hospital mortality (4.5% vs. 1.1%, p< 0.001), sepsis (3.2% vs. 1.9%, p< 0.001), acute kidney injury (21.2% vs. 12.1%, p< 0.001) (AKI), intensive care unit (ICU) admission (5.2% vs. 2.3%, p< 0.001) and DVT (3.9% vs. 1.8%, p< 0.001). After adjusting for confounding factors, patients with malnutrition had a higher risk of mortality (adjusted odds ratio-2.08; p< 0.001) compared to patients without malnutrition. Patients with malnutrition also had a statistically significant longer LOS (3 days; p< 0.001) and higher THC ($22,252; p< 0.001) compared to patients without malnutrition.
Discussion: Patients with CD and malnutrition are at high risk of worse outcomes. Early identification of malnutrition in CD can help predict morbidity and mortality. Strict adherence to a gluten-free diet can prevent Malnutrition. Further studies identifying factors associated with malnutrition in CD and the impact of early interventions to prevent and treat malnutrition are encouraged.

Disclosures:
Kanwal Bains, MBBS, CNSC1, Aalam Sohal, MD2, Hunza Chaudhry, MD3, Ishandeep Singh, MBBS4, Shivam Kalra, MBBS5, Dino Dukovic, BS6, Avin Aggarwal, MBBS7. P4105 - Impact of Malnutrition in Patients Hospitalized With Celiac Disease: Analysis of National Inpatient Sample 2016-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona, Tucson, AZ; 2Liver Institute Northwest, Seattle, WA; 3University of California San Francisco, Fresno, CA; 4Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 5Trident Medical Center, Charleston, SC; 6Ross University School of Medicine, Maramar, FL; 7University of Arizona College of Medicine, Tucson, AZ
Introduction: Celiac disease (CD) is a T cell-mediated gluten sensitivity that results in villous atrophy in the small intestine leading to chronic malabsorption. Although malnutrition is a known complication in patients with CD, its impact on outcomes is unknown. We assessed the impact of malnutrition on in-hospital outcomes in patients with CD.
Methods: National Inpatient Sample 2016-2020 was used to identify adult patients with a primary discharge diagnosis of CD. Patients with missing demographics or mortality were excluded from the analysis. Data were collected on patient demographics, hospital characteristics, Charlson Comorbidity Index (CCI), and Charlson comorbidities. We compared the incidence of outcomes, including mortality, deep vein thrombosis (DVT), sepsis, acute kidney injury (AKI), intensive care unit(ICU) admission, length of stay (LOS), and total hospitalization charges (THC) between the two groups. The relationship between mortality, LOS, and total hospitalization charges was analyzed using the multivariate regression model.
Results: A total of 187,310 patients with CD were included in the analysis. Of these, 15,555 (8.3%) patients were malnourished. The majority of the patients in the malnourished group were elderly > 65 yrs age (53.1%), female (66.3%), had Medicare (60.14%), and were in the highest income quartile (27.9%). The incidence of in-hospital mortality (4.5% vs. 1.1%, p< 0.001), sepsis (3.2% vs. 1.9%, p< 0.001), acute kidney injury (21.2% vs. 12.1%, p< 0.001) (AKI), intensive care unit (ICU) admission (5.2% vs. 2.3%, p< 0.001) and DVT (3.9% vs. 1.8%, p< 0.001). After adjusting for confounding factors, patients with malnutrition had a higher risk of mortality (adjusted odds ratio-2.08; p< 0.001) compared to patients without malnutrition. Patients with malnutrition also had a statistically significant longer LOS (3 days; p< 0.001) and higher THC ($22,252; p< 0.001) compared to patients without malnutrition.
Discussion: Patients with CD and malnutrition are at high risk of worse outcomes. Early identification of malnutrition in CD can help predict morbidity and mortality. Strict adherence to a gluten-free diet can prevent Malnutrition. Further studies identifying factors associated with malnutrition in CD and the impact of early interventions to prevent and treat malnutrition are encouraged.

Figure: Outcomes, stratified by the presence of malnutrition
Disclosures:
Kanwal Bains indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Hunza Chaudhry indicated no relevant financial relationships.
Ishandeep Singh indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Dino Dukovic indicated no relevant financial relationships.
Avin Aggarwal indicated no relevant financial relationships.
Kanwal Bains, MBBS, CNSC1, Aalam Sohal, MD2, Hunza Chaudhry, MD3, Ishandeep Singh, MBBS4, Shivam Kalra, MBBS5, Dino Dukovic, BS6, Avin Aggarwal, MBBS7. P4105 - Impact of Malnutrition in Patients Hospitalized With Celiac Disease: Analysis of National Inpatient Sample 2016-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
