Tuesday Poster Session
Category: Colon
P3105 - Eosinophilic Gastrointestinal Disease Associated with Allergic Bronchopulmonary Aspergillosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Katelin Durham, MD
University of Iowa Hospitals & Clinics
Iowa City, IA
Presenting Author(s)
Katelin Durham, MD, Vijayvardhan Kamalumpundi, BS, Xiaocen Zhang, MD
University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Allergic bronchopulmonary aspergillosis (ABPA) is a pulmonary disease caused by hypersensitivity reaction to Aspergillus fumigatus and is associated with the presence of elevated blood eosinophils and serum IgE. ABPA is not known to cause eosinophilic infiltration within the gastrointestinal tract. We report a rare case of eosinophilic gastrointestinal disease (EGID) in a patient with ABPA.
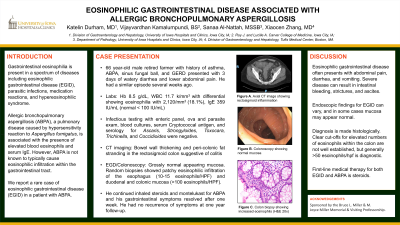
Case Description/Methods: A 66-year-old male retired farmer with history of asthma, ABPA, sinus fungal ball, and gastroesophageal reflux presented with a three-day history of watery diarrhea and lower abdominal pain. He had a similar episode several weeks prior. Labs on admission were remarkable for hemoglobin 8.5 g/dL and leukocyte count 11.7 k/mm3, with differential showing marked eosinophilia at 2,120/mm3 that was significantly increased from prior. Serum IgE was elevated at 359 IU/mL. Computed tomography imaging showed bowel wall thickening and peri-colonic fat stranding in the rectosigmoid colon suggestive of colitis. Infectious evaluation with enteric panel, ova and parasite exam, blood cultures, serum Cryptococcal antigen, and serology for Ascaris, Strongyloides, Toxocara, Trichinella, and Coccidioides were negative. Bidirectional endoscopy showed normal appearing esophagus, stomach, and mild erythema and edema of the duodenal mucosa. Terminal ileum and colon appeared grossly normal. Random biopsies demonstrated patchy eosinophilic infiltration of the esophageal epithelium (10-15 eosinophils/HPF) and duodenal and colonic mucosa ( >100 eosinophils/HPF). The patient was diagnosed with ABPA 12 years prior in setting of bronchiectasis, eosinophilia, elevated Aspergillus IgG and IgE, and positive skin testing. During hospitalization he continued on inhaled steroids and montelukast for ABPA. His gastrointestinal symptoms resolved after one week without additional treatment. He had no recurrence of symptoms at one-year follow up.
Discussion: Gastrointestinal eosinophilia is present in a spectrum of diseases including EGID, parasitic infections, medication reactions, and hypereosinophilic syndrome. To date, there has been only one case of ABPA contributing to gastrointestinal eosinophilia.1 Current hypotheses suggest that Aspergillus-mediated TH2 responses may promote eosinophilic infiltration of the intestinal wall. This can lead to intestinal bleeding, strictures, and ascites. First-line medical therapy for both EGID and ABPA is steroids.
Reference: 1. Bumbacea et al. Investig Allergol Clin Immunol. 2015.
Disclosures:
Katelin Durham, MD, Vijayvardhan Kamalumpundi, BS, Xiaocen Zhang, MD. P3105 - Eosinophilic Gastrointestinal Disease Associated with Allergic Bronchopulmonary Aspergillosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Allergic bronchopulmonary aspergillosis (ABPA) is a pulmonary disease caused by hypersensitivity reaction to Aspergillus fumigatus and is associated with the presence of elevated blood eosinophils and serum IgE. ABPA is not known to cause eosinophilic infiltration within the gastrointestinal tract. We report a rare case of eosinophilic gastrointestinal disease (EGID) in a patient with ABPA.
Case Description/Methods: A 66-year-old male retired farmer with history of asthma, ABPA, sinus fungal ball, and gastroesophageal reflux presented with a three-day history of watery diarrhea and lower abdominal pain. He had a similar episode several weeks prior. Labs on admission were remarkable for hemoglobin 8.5 g/dL and leukocyte count 11.7 k/mm3, with differential showing marked eosinophilia at 2,120/mm3 that was significantly increased from prior. Serum IgE was elevated at 359 IU/mL. Computed tomography imaging showed bowel wall thickening and peri-colonic fat stranding in the rectosigmoid colon suggestive of colitis. Infectious evaluation with enteric panel, ova and parasite exam, blood cultures, serum Cryptococcal antigen, and serology for Ascaris, Strongyloides, Toxocara, Trichinella, and Coccidioides were negative. Bidirectional endoscopy showed normal appearing esophagus, stomach, and mild erythema and edema of the duodenal mucosa. Terminal ileum and colon appeared grossly normal. Random biopsies demonstrated patchy eosinophilic infiltration of the esophageal epithelium (10-15 eosinophils/HPF) and duodenal and colonic mucosa ( >100 eosinophils/HPF). The patient was diagnosed with ABPA 12 years prior in setting of bronchiectasis, eosinophilia, elevated Aspergillus IgG and IgE, and positive skin testing. During hospitalization he continued on inhaled steroids and montelukast for ABPA. His gastrointestinal symptoms resolved after one week without additional treatment. He had no recurrence of symptoms at one-year follow up.
Discussion: Gastrointestinal eosinophilia is present in a spectrum of diseases including EGID, parasitic infections, medication reactions, and hypereosinophilic syndrome. To date, there has been only one case of ABPA contributing to gastrointestinal eosinophilia.1 Current hypotheses suggest that Aspergillus-mediated TH2 responses may promote eosinophilic infiltration of the intestinal wall. This can lead to intestinal bleeding, strictures, and ascites. First-line medical therapy for both EGID and ABPA is steroids.
Reference: 1. Bumbacea et al. Investig Allergol Clin Immunol. 2015.
Disclosures:
Katelin Durham indicated no relevant financial relationships.
Vijayvardhan Kamalumpundi indicated no relevant financial relationships.
Xiaocen Zhang indicated no relevant financial relationships.
Katelin Durham, MD, Vijayvardhan Kamalumpundi, BS, Xiaocen Zhang, MD. P3105 - Eosinophilic Gastrointestinal Disease Associated with Allergic Bronchopulmonary Aspergillosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

