Tuesday Poster Session
Category: Colon
P3106 - Post Colonoscopy Diverticulitis in an Ulcerative Colitis Patient Treated with Adalimumab
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Tyrell Daniel, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Tyrell Daniel, MD1, Alexandra Johnston, DO2
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Introduction: Colonic diverticulitis is inflammation secondary to microscopic or macroscopic perforation of diverticula. Risk factors are obesity, smoking, NSAID use. Post colonoscopy diverticulitis is rare with an estimated incidence of 0.04 - 0.08%. Given its rarity, there is no guideline to management. Here we present a case of a 69 year old female who presented with post-colonoscopy diverticulitis.
Case Description/Methods: A 69-year-old female with a seven year history of ulcerative proctosigmoiditis on adalimumab for 4 months for enteropathic arthritis per rheumatology presented as a transfer from an outside hospital (OSH) due to concerns for an ulcerative colitis (UC) flare versus diverticulitis. Two weeks prior to her presentation, she had a colonoscopy for iron deficiency anemia. Colonoscopy with biopsies revealed endoscopic and histologic remission of UC but diverticulosis in the sigmoid and ascending colon. Prior to her colonoscopy, she averaged two non-bloody bowel movements per day with her last bowel movement on the day of procedure. Two weeks later, she reported constipation and absent flatus. Her gastroenterologist recommended polyethylene glycol (PEG) twice per day. She developed progressive crampy abdominal pain in the left lower quadrant with non-bilious emesis. Three days later, she presented to the OSH for evaluation due to worsening symptoms. CT of the abdomen and pelvis noted acute sigmoid diverticulitis with moderate dilation of the proximal colon with stool and scattered air in diverticulum. She was transferred to our hospital for Gastroenterology evaluation. Upon transfer, she was febrile to 100.4 F, pulse 107, blood pressure 128/71 with tenderness in the left lower quadrant. Pertinent tests are in Table 1. Repeat CT showed sigmoid diverticulitis with antecolic and retrocolic gas containing abscesses. She was managed for diverticulitis with bowel rest, IV Ceftriaxone, IV Metronidazole, PEG with daily improvement in nausea, abdominal pain and bowel movements.
Discussion: Post colonoscopy diverticulitis is a rare complication of colonoscopy. We hypothesize that the risk of post colonoscopy diverticulitis may be increased in IBD patients with diverticulosis using tumor necrosis factor-alpha (TNF) inhibitors compared to IBD patients with diverticulosis without TNF inhibitor use. Hence more studies are needed to accurately estimate this risk. It is also important to counsel IBD patients on TNF inhibitors about the proposed increased infection risk with endoscopic interventions.

Disclosures:
Tyrell Daniel, MD1, Alexandra Johnston, DO2. P3106 - Post Colonoscopy Diverticulitis in an Ulcerative Colitis Patient Treated with Adalimumab, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Introduction: Colonic diverticulitis is inflammation secondary to microscopic or macroscopic perforation of diverticula. Risk factors are obesity, smoking, NSAID use. Post colonoscopy diverticulitis is rare with an estimated incidence of 0.04 - 0.08%. Given its rarity, there is no guideline to management. Here we present a case of a 69 year old female who presented with post-colonoscopy diverticulitis.
Case Description/Methods: A 69-year-old female with a seven year history of ulcerative proctosigmoiditis on adalimumab for 4 months for enteropathic arthritis per rheumatology presented as a transfer from an outside hospital (OSH) due to concerns for an ulcerative colitis (UC) flare versus diverticulitis. Two weeks prior to her presentation, she had a colonoscopy for iron deficiency anemia. Colonoscopy with biopsies revealed endoscopic and histologic remission of UC but diverticulosis in the sigmoid and ascending colon. Prior to her colonoscopy, she averaged two non-bloody bowel movements per day with her last bowel movement on the day of procedure. Two weeks later, she reported constipation and absent flatus. Her gastroenterologist recommended polyethylene glycol (PEG) twice per day. She developed progressive crampy abdominal pain in the left lower quadrant with non-bilious emesis. Three days later, she presented to the OSH for evaluation due to worsening symptoms. CT of the abdomen and pelvis noted acute sigmoid diverticulitis with moderate dilation of the proximal colon with stool and scattered air in diverticulum. She was transferred to our hospital for Gastroenterology evaluation. Upon transfer, she was febrile to 100.4 F, pulse 107, blood pressure 128/71 with tenderness in the left lower quadrant. Pertinent tests are in Table 1. Repeat CT showed sigmoid diverticulitis with antecolic and retrocolic gas containing abscesses. She was managed for diverticulitis with bowel rest, IV Ceftriaxone, IV Metronidazole, PEG with daily improvement in nausea, abdominal pain and bowel movements.
Discussion: Post colonoscopy diverticulitis is a rare complication of colonoscopy. We hypothesize that the risk of post colonoscopy diverticulitis may be increased in IBD patients with diverticulosis using tumor necrosis factor-alpha (TNF) inhibitors compared to IBD patients with diverticulosis without TNF inhibitor use. Hence more studies are needed to accurately estimate this risk. It is also important to counsel IBD patients on TNF inhibitors about the proposed increased infection risk with endoscopic interventions.

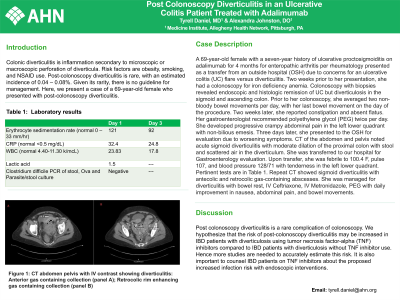
Figure: Figure 1: CT abdomen pelvis with IV contrast showing diverticulitis: Anterior gas containing collection (panel A); Retrocolic rim enhancing gas containing collection (panel B)
Disclosures:
Tyrell Daniel indicated no relevant financial relationships.
Alexandra Johnston indicated no relevant financial relationships.
Tyrell Daniel, MD1, Alexandra Johnston, DO2. P3106 - Post Colonoscopy Diverticulitis in an Ulcerative Colitis Patient Treated with Adalimumab, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
