Tuesday Poster Session
Category: Colon
P3107 - Fluoroquinolone-Induced Ischemic Colitis: A Case Series
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- BP
Blake Purtle, MD
University of Texas Health Science Center
Houston, TX
Presenting Author(s)
Blake Purtle, MD1, Keith Garrison, MD2, Abdullah Aleem, MD3, Suhair Al Salihi, MD1, Andrew W. DuPont, MD4
1University of Texas Health Science Center, Houston, TX; 2UT Houston, Houston, TX; 3University of Texas Health Science Center, Houston, AZ; 4University of Texas at Houston Medical School, Houston, TX
Introduction: Ischemic colitis is a common cause of acute lower gastrointestinal bleeding in the elderly with a reported incidence of 4% in this population1. Antibiotic-associated ischemic colitis is uncommon, which is typically right-sided and is thought to be due to an altered gut microbiome2. We present two cases of ciprofloxacin-induced ischemic colitis.
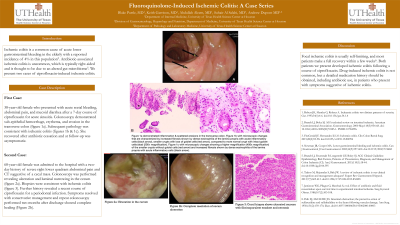
Case Description/Methods: 38-year-old female who presented with acute rectal bleeding, abdominal pain, and mucoid diarrhea after a 7-day course of ciprofloxacin for acute sinusitis. Colonoscopy demonstrated sub-epithelial hemorrhage, erythema, and erosion in the transverse colon (figure 1a). Subsequent pathology was consistent with ischemic colitis (figures 1b & 1c). She recovered after antibiotic cessation and at follow-up was asymptomatic.
68-year-old female was admitted to the hospital with a two-day history of severe right lower quadrant abdominal pain and CT suggestive of a cecal mass. Colonoscopy was performed revealing ulceration and luminal narrowing in the cecum (figure 1d). Biopsies were consistent with ischemic colitis (figure 1f). Further history revealed a recent course of ciprofloxacin for a periodontal infection. Symptoms resolved with conservative management and repeat colonoscopy performed two months after discharge showed complete healing (Figure 1e).
Discussion: Focal ischemic colitis is usually self-limiting, and most patients make a full recovery within a few weeks3. Both patients we present developed ischemic colitis following a course of ciprofloxacin. Drug-induced ischemic colitis is not common, but a detailed medication history should be obtained, including antibiotic use, in patients who present with symptoms suggestive of ischemic colitis.
1. Brandt LJ, Boley SJ. AGA technical review on intestinal ischemia. American Gastrointestinal Association. Gastroenterology. 2000 May;118(5):954-68. doi: 10.1016/s0016-5085(00)70183-1. PMID: 10784596.
2. Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ. ACG Clinical Guideline: Epidemiology, Risk Factors, Patterns of Presentation, Diagnosis, and Management of Colon Ischemia (CI). Am J Gastroenterol. 2015;110(1):18-44. doi:10.1038/ajg.2014.395
3. Tadros M, Majumder S, Birk JW. A review of ischemic colitis: is our clinical recognition and management adequate? Expert Rev Gastroenterol Hepatol. 2013;7(7):605-613. doi:10.1586/17474124.2013.832485

Disclosures:
Blake Purtle, MD1, Keith Garrison, MD2, Abdullah Aleem, MD3, Suhair Al Salihi, MD1, Andrew W. DuPont, MD4. P3107 - Fluoroquinolone-Induced Ischemic Colitis: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center, Houston, TX; 2UT Houston, Houston, TX; 3University of Texas Health Science Center, Houston, AZ; 4University of Texas at Houston Medical School, Houston, TX
Introduction: Ischemic colitis is a common cause of acute lower gastrointestinal bleeding in the elderly with a reported incidence of 4% in this population1. Antibiotic-associated ischemic colitis is uncommon, which is typically right-sided and is thought to be due to an altered gut microbiome2. We present two cases of ciprofloxacin-induced ischemic colitis.
Case Description/Methods: 38-year-old female who presented with acute rectal bleeding, abdominal pain, and mucoid diarrhea after a 7-day course of ciprofloxacin for acute sinusitis. Colonoscopy demonstrated sub-epithelial hemorrhage, erythema, and erosion in the transverse colon (figure 1a). Subsequent pathology was consistent with ischemic colitis (figures 1b & 1c). She recovered after antibiotic cessation and at follow-up was asymptomatic.
68-year-old female was admitted to the hospital with a two-day history of severe right lower quadrant abdominal pain and CT suggestive of a cecal mass. Colonoscopy was performed revealing ulceration and luminal narrowing in the cecum (figure 1d). Biopsies were consistent with ischemic colitis (figure 1f). Further history revealed a recent course of ciprofloxacin for a periodontal infection. Symptoms resolved with conservative management and repeat colonoscopy performed two months after discharge showed complete healing (Figure 1e).
Discussion: Focal ischemic colitis is usually self-limiting, and most patients make a full recovery within a few weeks3. Both patients we present developed ischemic colitis following a course of ciprofloxacin. Drug-induced ischemic colitis is not common, but a detailed medication history should be obtained, including antibiotic use, in patients who present with symptoms suggestive of ischemic colitis.
1. Brandt LJ, Boley SJ. AGA technical review on intestinal ischemia. American Gastrointestinal Association. Gastroenterology. 2000 May;118(5):954-68. doi: 10.1016/s0016-5085(00)70183-1. PMID: 10784596.
2. Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ. ACG Clinical Guideline: Epidemiology, Risk Factors, Patterns of Presentation, Diagnosis, and Management of Colon Ischemia (CI). Am J Gastroenterol. 2015;110(1):18-44. doi:10.1038/ajg.2014.395
3. Tadros M, Majumder S, Birk JW. A review of ischemic colitis: is our clinical recognition and management adequate? Expert Rev Gastroenterol Hepatol. 2013;7(7):605-613. doi:10.1586/17474124.2013.832485

Figure: Figure A demonstrated inflammation and scattered erosions in the transverse colon. Figure B with microscopic change that are characterized by increased fibrosis shown by dense eosinophilia of the lamina propria with acute inflammatory cells (black arrow), smaller crypts with loss of goblet cells (red arrow), compared to more normal crypt with intact goblet cells (star) (200x magnification). Figure C with microscopic changes showing a higher magnification (400x magnification) of the smaller crypts with goblet cells (red arrow) and increased fibrosis shown by dense eosinophilia of the lamina propria with acute inflammatory cells (black arrow).
Figure D: Ulceration in the cecum
Figure E: Complete resolution of cecum ulceration
Figure F: Cecal biopsy shows ulcerated mucosa with fibrinopurulent exudate and necrosis.
Figure D: Ulceration in the cecum
Figure E: Complete resolution of cecum ulceration
Figure F: Cecal biopsy shows ulcerated mucosa with fibrinopurulent exudate and necrosis.
Disclosures:
Blake Purtle indicated no relevant financial relationships.
Keith Garrison indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
Suhair Al Salihi indicated no relevant financial relationships.
Andrew DuPont indicated no relevant financial relationships.
Blake Purtle, MD1, Keith Garrison, MD2, Abdullah Aleem, MD3, Suhair Al Salihi, MD1, Andrew W. DuPont, MD4. P3107 - Fluoroquinolone-Induced Ischemic Colitis: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
