Tuesday Poster Session
Category: Small Intestine
P4109 - Serologic Confirmed Celiac Disease Patients Are at Elevated Risk for Peptic Ulcer Disease: A Nation-Wide Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Rama Nanah, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Rama Nanah, MD1, Arjun Chatterjee, MD2, Jehad Almasri, MD, MSc3, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, Claire Jansson-Knodell, MD1, Alberto Rubio-Tapia, MD2
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3University of Cincinnati, Cincinnati, OH
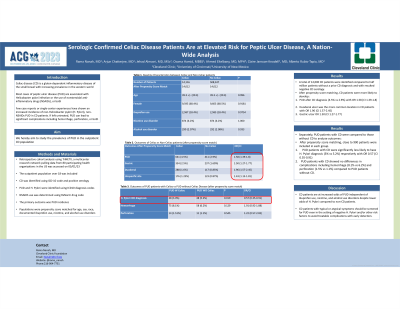
Introduction: Celiac disease (CD) is a gluten-dependent inflammatory disease of the small bowel with increasing prevalence in the western world. Most cases of peptic ulcer disease (PUD) are associated with Helicobacter pylori infection or the use of nonsteroidal anti-inflammatory drugs (NSAIDs), or both . Few case reports or single-center experiences have shown an increased incidence of non-Helicobacter pylori (H. Pylori), non-NSAIDs PUD in CD patients. If left untreated, PUD can lead to significant complications including hemorrhage, perforation, or both. We hereby aim to study the prevalence of PUD in the outpatient CD population.
Methods: TriNETX, a multicenter research network pulling data from 80 participating health organizations in the US was accessed on 05/01/23. The outpatient population over 18 was included. CD was identified using ICD-10 code and positive serology. PUD and H. Pylori were identified using ICD-10 diagnosis codes. NSAIDS use was determined using RxNorm drug code. The primary outcome was PUD incidence.
Results: A total of 14,116 CD patients were identified compared to 508,347 patients without a prior CD diagnosis and with resulted negative CD serology. Populations were propensity score matched for age, sex, race, documented ibuprofen use, nicotine, and alcohol use disorders. After propensity score matching, CD patients were more likely to develop PUD after CD diagnosis (4.5% vs 2.9%) with OR 1.58 (CI 1.39-1.8) compared to non-CD patients. Duodenal ulcer was the more common location in CD patients with OR 1.96 (CI 1.57-2.45) compared to gastric ulcer OR 1.50 (CI 1.27-1.77).
Separately, PUD patients with CD were compared to those without CD to analyze outcomes. After propensity score matching for age, sex, race, documented ibuprofen use, nicotine, and alcohol use disorders, 923 patients were included in each group. PUD patients with CD were significantly less likely to have H. Pylori diagnosis (3% vs 5.2%) respectively with OR 0.57 (CI 0.35-0.91). PUD patients with CD showed no differences in complications including hemorrhage (8.1% vs 6.2%) and perforation (1.5% vs 1.1%) compared to PUD patients without CD.
Discussion: CD patients are at increased odds of PUD independent of ibuprofen use, nicotine, and alcohol use disorders despite lower odds of H. Pylori compared to non-CD patients. CD patients with typical or atypical symptoms should be screened for PUD even in the setting of negative H. Pylori and/or other risk factors to avoid treatable complications with early detection.
Disclosures:
Rama Nanah, MD1, Arjun Chatterjee, MD2, Jehad Almasri, MD, MSc3, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, Claire Jansson-Knodell, MD1, Alberto Rubio-Tapia, MD2. P4109 - Serologic Confirmed Celiac Disease Patients Are at Elevated Risk for Peptic Ulcer Disease: A Nation-Wide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3University of Cincinnati, Cincinnati, OH
Introduction: Celiac disease (CD) is a gluten-dependent inflammatory disease of the small bowel with increasing prevalence in the western world. Most cases of peptic ulcer disease (PUD) are associated with Helicobacter pylori infection or the use of nonsteroidal anti-inflammatory drugs (NSAIDs), or both . Few case reports or single-center experiences have shown an increased incidence of non-Helicobacter pylori (H. Pylori), non-NSAIDs PUD in CD patients. If left untreated, PUD can lead to significant complications including hemorrhage, perforation, or both. We hereby aim to study the prevalence of PUD in the outpatient CD population.
Methods: TriNETX, a multicenter research network pulling data from 80 participating health organizations in the US was accessed on 05/01/23. The outpatient population over 18 was included. CD was identified using ICD-10 code and positive serology. PUD and H. Pylori were identified using ICD-10 diagnosis codes. NSAIDS use was determined using RxNorm drug code. The primary outcome was PUD incidence.
Results: A total of 14,116 CD patients were identified compared to 508,347 patients without a prior CD diagnosis and with resulted negative CD serology. Populations were propensity score matched for age, sex, race, documented ibuprofen use, nicotine, and alcohol use disorders. After propensity score matching, CD patients were more likely to develop PUD after CD diagnosis (4.5% vs 2.9%) with OR 1.58 (CI 1.39-1.8) compared to non-CD patients. Duodenal ulcer was the more common location in CD patients with OR 1.96 (CI 1.57-2.45) compared to gastric ulcer OR 1.50 (CI 1.27-1.77).
Separately, PUD patients with CD were compared to those without CD to analyze outcomes. After propensity score matching for age, sex, race, documented ibuprofen use, nicotine, and alcohol use disorders, 923 patients were included in each group. PUD patients with CD were significantly less likely to have H. Pylori diagnosis (3% vs 5.2%) respectively with OR 0.57 (CI 0.35-0.91). PUD patients with CD showed no differences in complications including hemorrhage (8.1% vs 6.2%) and perforation (1.5% vs 1.1%) compared to PUD patients without CD.
Discussion: CD patients are at increased odds of PUD independent of ibuprofen use, nicotine, and alcohol use disorders despite lower odds of H. Pylori compared to non-CD patients. CD patients with typical or atypical symptoms should be screened for PUD even in the setting of negative H. Pylori and/or other risk factors to avoid treatable complications with early detection.
Disclosures:
Rama Nanah indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Jehad Almasri indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Ahmed Eltelbany indicated no relevant financial relationships.
Claire Jansson-Knodell: ClearPoint Neuro – Stock-publicly held company(excluding mutual/index funds). DarioHealth – Stock-publicly held company(excluding mutual/index funds). DermTech – Stock-publicly held company(excluding mutual/index funds). DiaMedica Therapeutics – Stock-publicly held company(excluding mutual/index funds). Exact Sciences – Stock-publicly held company(excluding mutual/index funds). Inari Medical – Stock-publicly held company(excluding mutual/index funds). Nano-X Imaging – Stock-publicly held company(excluding mutual/index funds). Outset Medical – Stock-publicly held company(excluding mutual/index funds). PavMed – Stock-publicly held company(excluding mutual/index funds). Takeda - AGA Research Scholars Award – Grant/Research Support. Transmedics – Stock-publicly held company(excluding mutual/index funds).
Alberto Rubio-Tapia indicated no relevant financial relationships.
Rama Nanah, MD1, Arjun Chatterjee, MD2, Jehad Almasri, MD, MSc3, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, Claire Jansson-Knodell, MD1, Alberto Rubio-Tapia, MD2. P4109 - Serologic Confirmed Celiac Disease Patients Are at Elevated Risk for Peptic Ulcer Disease: A Nation-Wide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
