Tuesday Poster Session
Category: Colon
P3128 - A Rare Cause of Hematochezia: Appendiceal Bleeding
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Patrick T. Magahis, BA
Weill Cornell Medicine
New York, NY
Presenting Author(s)
Patrick T.. Magahis, BA1, Aiya Aboubakr, MD2, David Wan, BS, MD1
1Weill Cornell Medicine, New York, NY; 2New York Presbyterian-Weill Cornell Medical Center, New York, NY
Introduction: Acute lower gastrointestinal bleeding (LGIB) from appendiceal hemorrhage is rare but must be considered in the differential diagnosis for hematochezia, given lack of endoscopic therapeutics and the need for timely surgical intervention. We present a rare case of LGIB from an appendiceal lesion that was diagnosed after several inconclusive endoscopic evaluations and ultimately treated successfully with surgical resection.
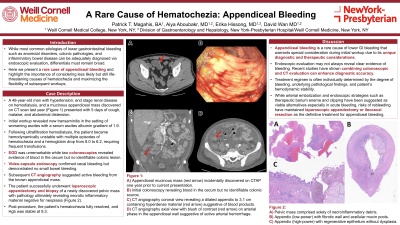
Case Description/Methods: A 48-year-old man with hypertension, end stage renal disease on hemodialysis, and mucinous appendiceal mass discovered on computed tomography (CT) scan last year (Figure 1) presented with signs of volume overload and his course was complicated by large volume hematochezia with vital sign changes and blood transfusion requirement. Given concern for massive upper GI bleeding, urgent esophagogastroduodenoscopy was performed but was unremarkable. Subsequent colonoscopy revealed blood in the right colon without identifiable active bleeding or mucosal abnormality. Repeat colonoscopy was done, given concern for question of poor prep impairing mucosal visualization and similarly identified red blood by cecal area, without active bleeding during exam. Video-capsule endoscopy was performed to rule out small bowel pathology and showed normal small bowel but red blood in the cecum. CT angiography performed next day showed active bleeding from the appendix. The patient successfully underwent laparoscopic appendectomy and biopsy of a newly discovered pelvic mass with pathology ultimately revealing necrotic inflammatory material negative for neoplasia. Post-procedure, the patient’s hematochezia fully resolved and hemoglobin was stable.
Discussion: Appendiceal bleeding is a rare cause of LGIB that warrants special consideration during initial workup due to its unique diagnostic and therapeutic considerations. As in our patient, endoscopic evaluation may not always reveal clear evidence of bleeding. Recent studies have shown that combining colonoscopy and CT evaluation can enhance diagnostic accuracy. Treatment regimen is often individually determined by the degree of bleeding, underlying pathological findings, and patient’s hemodynamic stability. While arterial embolization and endoscopic strategies such as therapeutic barium enema and clipping have been suggested as viable alternatives especially in acute cases, risks of rebleeding have maintained laparoscopic appendectomy or ileocecal resection as the definitive treatment of choice for appendiceal bleeding.

Disclosures:
Patrick T.. Magahis, BA1, Aiya Aboubakr, MD2, David Wan, BS, MD1. P3128 - A Rare Cause of Hematochezia: Appendiceal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Weill Cornell Medicine, New York, NY; 2New York Presbyterian-Weill Cornell Medical Center, New York, NY
Introduction: Acute lower gastrointestinal bleeding (LGIB) from appendiceal hemorrhage is rare but must be considered in the differential diagnosis for hematochezia, given lack of endoscopic therapeutics and the need for timely surgical intervention. We present a rare case of LGIB from an appendiceal lesion that was diagnosed after several inconclusive endoscopic evaluations and ultimately treated successfully with surgical resection.
Case Description/Methods: A 48-year-old man with hypertension, end stage renal disease on hemodialysis, and mucinous appendiceal mass discovered on computed tomography (CT) scan last year (Figure 1) presented with signs of volume overload and his course was complicated by large volume hematochezia with vital sign changes and blood transfusion requirement. Given concern for massive upper GI bleeding, urgent esophagogastroduodenoscopy was performed but was unremarkable. Subsequent colonoscopy revealed blood in the right colon without identifiable active bleeding or mucosal abnormality. Repeat colonoscopy was done, given concern for question of poor prep impairing mucosal visualization and similarly identified red blood by cecal area, without active bleeding during exam. Video-capsule endoscopy was performed to rule out small bowel pathology and showed normal small bowel but red blood in the cecum. CT angiography performed next day showed active bleeding from the appendix. The patient successfully underwent laparoscopic appendectomy and biopsy of a newly discovered pelvic mass with pathology ultimately revealing necrotic inflammatory material negative for neoplasia. Post-procedure, the patient’s hematochezia fully resolved and hemoglobin was stable.
Discussion: Appendiceal bleeding is a rare cause of LGIB that warrants special consideration during initial workup due to its unique diagnostic and therapeutic considerations. As in our patient, endoscopic evaluation may not always reveal clear evidence of bleeding. Recent studies have shown that combining colonoscopy and CT evaluation can enhance diagnostic accuracy. Treatment regimen is often individually determined by the degree of bleeding, underlying pathological findings, and patient’s hemodynamic stability. While arterial embolization and endoscopic strategies such as therapeutic barium enema and clipping have been suggested as viable alternatives especially in acute cases, risks of rebleeding have maintained laparoscopic appendectomy or ileocecal resection as the definitive treatment of choice for appendiceal bleeding.

Figure: Figure 1: A) Appendiceal mucinous mass (red arrow) incidentally discovered on CT abdomen and pelvis one year prior to current presentation; B) Initial colonoscopy revealing blood in the cecum but no identifiable colonic source; C) CT angiography coronal view revealing a dilated appendix to 3.1 cm containing hyperdense material (red arrow) suggestive of blood products; and D) CT angiography axial view with blush of contrast (red arrow) on arterial phase in the appendiceal wall suggestive of active arterial hemorrhage.
Disclosures:
Patrick Magahis indicated no relevant financial relationships.
Aiya Aboubakr indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Patrick T.. Magahis, BA1, Aiya Aboubakr, MD2, David Wan, BS, MD1. P3128 - A Rare Cause of Hematochezia: Appendiceal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
