Tuesday Poster Session
Category: Small Intestine
P4129 - Sclerosing Mesenteritis: A Rare Cause of Abdominal Pain
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- PM
Patrick McCarthy, MD
University of Maryland School of Medicine
Baltimore, MD
Presenting Author(s)
Patrick McCarthy, MD, Kelvin Liao, MD, Kiran Motwani, MD, Kirti Shetty, MD
University of Maryland School of Medicine, Baltimore, MD
Introduction: Sclerosing mesenteritis is a rare condition that occurs when the mesentery becomes inflamed, causing extrinsic compression of the small intestine, subsequent luminal narrowing and obstruction. Given the nonspecific symptoms, sclerosing mesenteritis can go undiagnosed until serious complications arise.
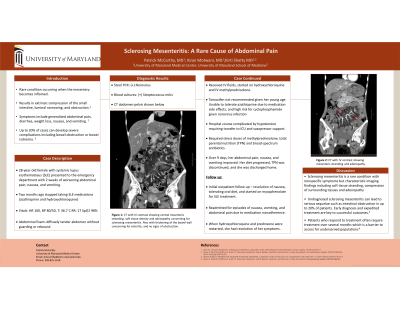
Case Description/Methods: A 28-year-old female with a history of systemic lupus erythematosus (SLE) presented to the emergency department with two weeks of worsening abdominal pain, nausea, and vomiting. She had stopped taking her SLE medications including azathioprine and hydroxychloroquine two months previously. A computerized tomography (CT) scan of her abdomen central mesenteric stranding, soft tissue density and adenopathy concerning for sclerosing mesenteritis. She was admitted and started on hydroxychloroquine and intravenous methylprednisolone. Tamoxifen was not recommended given her young age, she was unable to tolerate azathioprine due to medication side effects, and her condition was compounded by norovirus infection making her high risk for cyclophosphamide. Her hospital course was complicated by hypotension requiring transfer to the intensive care unit and vasopressor support. Repeat abdominal CT scan showed thickening of the bowel wall concerning for enteritis, and no signs of obstruction and blood cultures grew streptococcus mitis, attributed to bacterial translocation, exacerbated by lack of oral intake and sclerosing mesenteritis. She required stress doses of methylprednisolone, total parental nutrition (TPN) and broad-spectrum antibiotics. Over 9 days, her abdominal pain, nausea, and vomiting improved. Her diet progressed, TPN was discontinued, and she was discharged home. At her outpatient follow up she had resolution of her nausea, was tolerating an oral diet, and was started on mycophenolate for SLE treatment.
Discussion: Sclerosing mesenteritis is a rare condition with nonspecific symptoms but very characteristic imaging findings which include soft tissue stranding and adenopathy. The underlying pathophysiology is unknown but is often associated with autoimmune conditions, in this case SLE, inflammatory bowel disease and lymphoma. Accurate diagnosis is based on having a high index of suspicion. Since undiagnosed sclerosing mesenteritis can lead to serious sequelae such as intestinal obstruction, early diagnosis and expedited treatment are key to successful outcomes.
Disclosures:
Patrick McCarthy, MD, Kelvin Liao, MD, Kiran Motwani, MD, Kirti Shetty, MD. P4129 - Sclerosing Mesenteritis: A Rare Cause of Abdominal Pain, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Maryland School of Medicine, Baltimore, MD
Introduction: Sclerosing mesenteritis is a rare condition that occurs when the mesentery becomes inflamed, causing extrinsic compression of the small intestine, subsequent luminal narrowing and obstruction. Given the nonspecific symptoms, sclerosing mesenteritis can go undiagnosed until serious complications arise.
Case Description/Methods: A 28-year-old female with a history of systemic lupus erythematosus (SLE) presented to the emergency department with two weeks of worsening abdominal pain, nausea, and vomiting. She had stopped taking her SLE medications including azathioprine and hydroxychloroquine two months previously. A computerized tomography (CT) scan of her abdomen central mesenteric stranding, soft tissue density and adenopathy concerning for sclerosing mesenteritis. She was admitted and started on hydroxychloroquine and intravenous methylprednisolone. Tamoxifen was not recommended given her young age, she was unable to tolerate azathioprine due to medication side effects, and her condition was compounded by norovirus infection making her high risk for cyclophosphamide. Her hospital course was complicated by hypotension requiring transfer to the intensive care unit and vasopressor support. Repeat abdominal CT scan showed thickening of the bowel wall concerning for enteritis, and no signs of obstruction and blood cultures grew streptococcus mitis, attributed to bacterial translocation, exacerbated by lack of oral intake and sclerosing mesenteritis. She required stress doses of methylprednisolone, total parental nutrition (TPN) and broad-spectrum antibiotics. Over 9 days, her abdominal pain, nausea, and vomiting improved. Her diet progressed, TPN was discontinued, and she was discharged home. At her outpatient follow up she had resolution of her nausea, was tolerating an oral diet, and was started on mycophenolate for SLE treatment.
Discussion: Sclerosing mesenteritis is a rare condition with nonspecific symptoms but very characteristic imaging findings which include soft tissue stranding and adenopathy. The underlying pathophysiology is unknown but is often associated with autoimmune conditions, in this case SLE, inflammatory bowel disease and lymphoma. Accurate diagnosis is based on having a high index of suspicion. Since undiagnosed sclerosing mesenteritis can lead to serious sequelae such as intestinal obstruction, early diagnosis and expedited treatment are key to successful outcomes.
Disclosures:
Patrick McCarthy indicated no relevant financial relationships.
Kelvin Liao indicated no relevant financial relationships.
Kiran Motwani indicated no relevant financial relationships.
Kirti Shetty: Glycotest – Grant/Research Support. HANMI - TRIA – Grant/Research Support. Lipocine – Grant/Research Support. Ocera – Grant/Research Support.
Patrick McCarthy, MD, Kelvin Liao, MD, Kiran Motwani, MD, Kirti Shetty, MD. P4129 - Sclerosing Mesenteritis: A Rare Cause of Abdominal Pain, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
