Tuesday Poster Session
Category: Small Intestine
P4136 - Death Awaits a Daring Duodenal Diverticulum
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- BK
Bradley Kapten, MD
Michigan State University/Ascension Providence - Providence Park Hospital
Farmington, MI
Presenting Author(s)
Bradley Kapten, MD1, Brandon Wiggins, DO, MPH2, Ruona Ebiai, MD3, Alan Cutler, MD4
1Michigan State University/Ascension Providence - Providence Park Hospital, Farmington Hills, MI; 2Ascension Genesys Hospital, Grand Blanc, MI; 3Ochsner Clinic Foundation, New Orleans, LA; 4Michigan State University/Ascension Providence - Providence Park Hospital, Southfield, MI
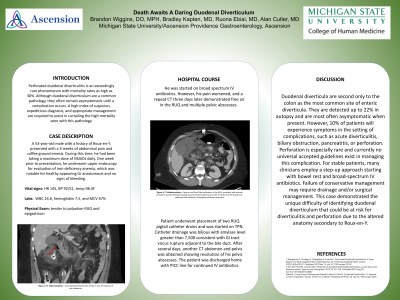
Introduction: Perforated duodenal diverticulitis is an exceedingly rare phenomenon with mortality rates as high as 30%. Although duodenal diverticulum are a common pathology, they often remain asymptomatic until a complication occurs. A high index of suspicion, expeditious diagnosis, and appropriate management are required to assist in curtailing the high mortality seen with this pathology.
Case Description/Methods: A 53-year-old male with a history of Roux-en-y, presented with 3-weeks of abdominal pain and coffee ground emesis. During this time, he had been taking a maximum dose of NSAIDs daily. One week prior to presentation, he underwent upper endoscopy for evaluation of iron deficiency anemia, which was notable for healthy appearing GJ anastomosis and no signs of bleeding.
Vital signs were notable for tachycardia and hypotension. Laboratory findings were remarkable for WBC 24.6, hemoglobin 7.5, and MCV 67%. On physical exam, he was tender to palpation in his RUQ and epigastrium. CT abdomen/pelvis revealed uncomplicated diverticulitis of the 1st and 2nd portions of the duodenum. He was started on broad spectrum IV antibiotics. However, his pain worsened and a repeat CT three days later demonstrated free air in the RUQ and multiple pelvic abscesses.
Patient underwent placement of two RUQ pigtail catheter drains and was started on TPN. Catheter drainage was bilious with amylase level greater than 7,500 consistent with GI tract viscus rupture adjacent to the bile duct. After several days, another CT abdomen and pelvis was obtained showing resolution of his pelvic abscesses. The patient was discharged home with PICC line for continued IV antibiotics.
Discussion: Duodenal diverticula are second only to the colon as the most common site of enteric diverticula. They are detected up to 22% in autopsy and are most often asymptomatic when present. However, 10% of patients will experience symptoms in the setting of complications, such as acute diverticulitis, biliary obstruction, pancreatitis, or perforation. Perforation is especially rare and currently no universal accepted guidelines exist in managing this complication. For stable patients, many clinicians employ a step up approach starting with bowel rest and broad spectrum IV antibiotics. Failure of conservative management may require drainage and/or surgical management. This case demonstrated the unique difficulty of identifying duodenal diverticulum that could be at risk for diverticulitis and perforation due to the altered anatomy secondary to roux en y.
Disclosures:
Bradley Kapten, MD1, Brandon Wiggins, DO, MPH2, Ruona Ebiai, MD3, Alan Cutler, MD4. P4136 - Death Awaits a Daring Duodenal Diverticulum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Michigan State University/Ascension Providence - Providence Park Hospital, Farmington Hills, MI; 2Ascension Genesys Hospital, Grand Blanc, MI; 3Ochsner Clinic Foundation, New Orleans, LA; 4Michigan State University/Ascension Providence - Providence Park Hospital, Southfield, MI
Introduction: Perforated duodenal diverticulitis is an exceedingly rare phenomenon with mortality rates as high as 30%. Although duodenal diverticulum are a common pathology, they often remain asymptomatic until a complication occurs. A high index of suspicion, expeditious diagnosis, and appropriate management are required to assist in curtailing the high mortality seen with this pathology.
Case Description/Methods: A 53-year-old male with a history of Roux-en-y, presented with 3-weeks of abdominal pain and coffee ground emesis. During this time, he had been taking a maximum dose of NSAIDs daily. One week prior to presentation, he underwent upper endoscopy for evaluation of iron deficiency anemia, which was notable for healthy appearing GJ anastomosis and no signs of bleeding.
Vital signs were notable for tachycardia and hypotension. Laboratory findings were remarkable for WBC 24.6, hemoglobin 7.5, and MCV 67%. On physical exam, he was tender to palpation in his RUQ and epigastrium. CT abdomen/pelvis revealed uncomplicated diverticulitis of the 1st and 2nd portions of the duodenum. He was started on broad spectrum IV antibiotics. However, his pain worsened and a repeat CT three days later demonstrated free air in the RUQ and multiple pelvic abscesses.
Patient underwent placement of two RUQ pigtail catheter drains and was started on TPN. Catheter drainage was bilious with amylase level greater than 7,500 consistent with GI tract viscus rupture adjacent to the bile duct. After several days, another CT abdomen and pelvis was obtained showing resolution of his pelvic abscesses. The patient was discharged home with PICC line for continued IV antibiotics.
Discussion: Duodenal diverticula are second only to the colon as the most common site of enteric diverticula. They are detected up to 22% in autopsy and are most often asymptomatic when present. However, 10% of patients will experience symptoms in the setting of complications, such as acute diverticulitis, biliary obstruction, pancreatitis, or perforation. Perforation is especially rare and currently no universal accepted guidelines exist in managing this complication. For stable patients, many clinicians employ a step up approach starting with bowel rest and broad spectrum IV antibiotics. Failure of conservative management may require drainage and/or surgical management. This case demonstrated the unique difficulty of identifying duodenal diverticulum that could be at risk for diverticulitis and perforation due to the altered anatomy secondary to roux en y.
Disclosures:
Bradley Kapten indicated no relevant financial relationships.
Brandon Wiggins indicated no relevant financial relationships.
Ruona Ebiai indicated no relevant financial relationships.
Alan Cutler indicated no relevant financial relationships.
Bradley Kapten, MD1, Brandon Wiggins, DO, MPH2, Ruona Ebiai, MD3, Alan Cutler, MD4. P4136 - Death Awaits a Daring Duodenal Diverticulum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
