Tuesday Poster Session
Category: Colon
P3138 - Did It Really Grow That Fast? A Large Cecal Lesion Just 6 Months After a Normal Screening Colonoscopy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- FW
Fazl Rahim Wazeen, MD
Greater Baltimore Medical Center
Towson, MD
Presenting Author(s)
Fazl Rahim Wazeen, MD1, Azfar Niazi, MD1, Syed Murtaza Haider Zaidi, MD2, Jayashrei Sairam, MD1, Akshay Duddu, MD1, Fatima Wazin, MBBS3, Ayesha Khan, MD1, Isra Amjed, MD1, Niraj Jani, MD4
1Greater Baltimore Medical Center, Towson, MD; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3King Edward Medical University, Towson, MD; 4Greater Baltimore Medical Center, Baltimore, MD
Introduction: ØPrimary colonic lymphoma (PCL) is an extremely rare
malignancy accounting for less than 0.3% of all colorectal malignancies. It is a challenging diagnosis due to its rarity and overlapping clinical presentation with other colonic diseases.
ØNon-Hodgkin lymphoma (NHL) is the most prevalent
subtype of lymphoma in the colon. Although the
gastrointestinal (GI) tract is the most predominant site for secondary lymphoma spread, primary lymphomas of the GI tract make up only 1-4% of all lymphomas.
Case Description/Methods: ØA 51-year-old female patient with a PMHx of GERD, presented for routine age-appropriate screening colonoscopy that was unremarkable.
Ø4 months later, she presented to the GI clinic with a constellation of abdominal cramping, diarrhea, off and on fever, and weight loss of 10 lbs.
ØCT AP with contrast showed moderate bowel wall thickening involving the ascending colon, suggestive of colitis.
Ø2 months later: diagnostic colonoscopy revealed an infiltrative, ulcerated, and partially obstructing large mass in the cecum, Biopsies revealed an atypical lymphoid infiltrate consistent with CD10-negative diffuse large B-cell lymphoma.
ØFISH revealed loss of the MYC gene region on chromosome 8q or monosomy of chromosome 8 and hyperintensity on PET CT in the ascending colon.
Ø2 weeks later, the patient was admitted to the ED with abdominal pain and was found to have a partial small bowel obstruction for which she was managed conservatively and was started on her first cycle of R-CHOP.
ØFollowing 2 cycles of R-CHOP, she presented again with recurrent intestinal obstruction for which she had laparoscopic right colectomy with ileo-transverse. Surgical pathology showed no residual lymphoma.
ØShe completed R-CHOP 7 cyles of R-CHOP. Repeat PET-CT post-treatment showed no evidence of residue or recurrent lymphoma with no recurrence of her lymphoma to date.
Discussion: ØPrimary colonic lymphomas account for less than 0.3 % of all large bowel malignancies. presents as abdominal pain, or GI bleed, a mass lesion, mimicking adenocarcinoma, or as multiple nodules resembling inflammatory bowel disease or diverticulitis.
Ø Risk factors: IBD, immunosuppression due to history of transplant or human (HIV).
ØPrognosis: Outcomes are dependent on both clinical features and pathologic aspects of DLBCL.
ØIn our case the patient was female, her symptoms rapidly progressed to cause bowel obstruction despite having an unremarkable screening Colonoscopy 6 months prior to her diagnostic colonoscopy.

Disclosures:
Fazl Rahim Wazeen, MD1, Azfar Niazi, MD1, Syed Murtaza Haider Zaidi, MD2, Jayashrei Sairam, MD1, Akshay Duddu, MD1, Fatima Wazin, MBBS3, Ayesha Khan, MD1, Isra Amjed, MD1, Niraj Jani, MD4. P3138 - Did It Really Grow That Fast? A Large Cecal Lesion Just 6 Months After a Normal Screening Colonoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Greater Baltimore Medical Center, Towson, MD; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3King Edward Medical University, Towson, MD; 4Greater Baltimore Medical Center, Baltimore, MD
Introduction: ØPrimary colonic lymphoma (PCL) is an extremely rare
malignancy accounting for less than 0.3% of all colorectal malignancies. It is a challenging diagnosis due to its rarity and overlapping clinical presentation with other colonic diseases.
ØNon-Hodgkin lymphoma (NHL) is the most prevalent
subtype of lymphoma in the colon. Although the
gastrointestinal (GI) tract is the most predominant site for secondary lymphoma spread, primary lymphomas of the GI tract make up only 1-4% of all lymphomas.
Case Description/Methods: ØA 51-year-old female patient with a PMHx of GERD, presented for routine age-appropriate screening colonoscopy that was unremarkable.
Ø4 months later, she presented to the GI clinic with a constellation of abdominal cramping, diarrhea, off and on fever, and weight loss of 10 lbs.
ØCT AP with contrast showed moderate bowel wall thickening involving the ascending colon, suggestive of colitis.
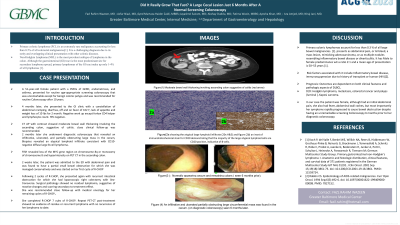
Ø2 months later: diagnostic colonoscopy revealed an infiltrative, ulcerated, and partially obstructing large mass in the cecum, Biopsies revealed an atypical lymphoid infiltrate consistent with CD10-negative diffuse large B-cell lymphoma.
ØFISH revealed loss of the MYC gene region on chromosome 8q or monosomy of chromosome 8 and hyperintensity on PET CT in the ascending colon.
Ø2 weeks later, the patient was admitted to the ED with abdominal pain and was found to have a partial small bowel obstruction for which she was managed conservatively and was started on her first cycle of R-CHOP.
ØFollowing 2 cycles of R-CHOP, she presented again with recurrent intestinal obstruction for which she had laparoscopic right colectomy with ileo-transverse. Surgical pathology showed no residual lymphoma.
ØShe completed R-CHOP 7 cyles of R-CHOP. Repeat PET-CT post-treatment showed no evidence of residue or recurrent lymphoma with no recurrence of her lymphoma to date.
Discussion: ØPrimary colonic lymphomas account for less than 0.3 % of all large bowel malignancies. presents as abdominal pain, or GI bleed, a mass lesion, mimicking adenocarcinoma, or as multiple nodules resembling inflammatory bowel disease or diverticulitis.
Ø Risk factors: IBD, immunosuppression due to history of transplant or human (HIV).
ØPrognosis: Outcomes are dependent on both clinical features and pathologic aspects of DLBCL.
ØIn our case the patient was female, her symptoms rapidly progressed to cause bowel obstruction despite having an unremarkable screening Colonoscopy 6 months prior to her diagnostic colonoscopy.

Figure: Figure (1)An infiltrative and ulcerated partially obstructing large circumferential mass was found in the cecum.
Disclosures:
Fazl Rahim Wazeen indicated no relevant financial relationships.
Azfar Niazi indicated no relevant financial relationships.
Syed Murtaza Haider Zaidi indicated no relevant financial relationships.
Jayashrei Sairam indicated no relevant financial relationships.
Akshay Duddu indicated no relevant financial relationships.
Fatima Wazin indicated no relevant financial relationships.
Ayesha Khan indicated no relevant financial relationships.
Isra Amjed indicated no relevant financial relationships.
Niraj Jani indicated no relevant financial relationships.
Fazl Rahim Wazeen, MD1, Azfar Niazi, MD1, Syed Murtaza Haider Zaidi, MD2, Jayashrei Sairam, MD1, Akshay Duddu, MD1, Fatima Wazin, MBBS3, Ayesha Khan, MD1, Isra Amjed, MD1, Niraj Jani, MD4. P3138 - Did It Really Grow That Fast? A Large Cecal Lesion Just 6 Months After a Normal Screening Colonoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
