Tuesday Poster Session
Category: Colon
P3142 - A Case of Herpes Simplex Virus Colitis in an Immunosuppressed Patient
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Jasmine Tidwell, MD
UConn Health
Farmington, CT
Presenting Author(s)
Jasmine Tidwell, MD, Minh Thu T. Nguyen, MD, Maryam Zenali, MD, Faripour Forouhar, MD, Campbell Stewart, MD, Roopjeet Bath, MD
UConn Health, Farmington, CT
Introduction: Herpes simplex virus (HSV) is a common virus capable of pathologies ranging from cold sores to colitis. When the gastrointestinal tract is involved, it usually affects the esophagus, perineum, and rectum. We describe a rare case of disseminated cutaneous HSV infection with concomitant colonic involvement in an immunosuppressed patient.
Case Description/Methods: A 48-year-old woman with a past medical history of systemic lupus erythematous previously complicated by pericardial effusion and lupus nephritis, presented due to a progressive rash. Her medications included mycophenolate mofetil 1 gram twice a day, voclosporin 23.7 mg twice daily, and prednisone 20 mg daily. The rash developed 10 days prior to admission, starting on her left buttock, then spreading to the pubic region, labia majora and perianal region. Skin viral swabs were positive for HSV type 2, which was confirmed with a punch biopsy. She was subsequently started on antiviral therapy.
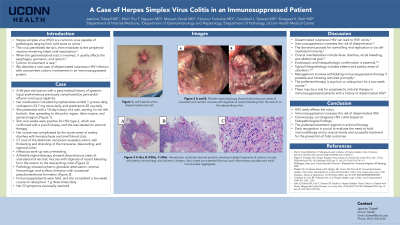
Her hospital course was complicated by acute onset of watery diarrhea with hematochezia and small blood clots. CT scan of the abdomen and pelvis revealed colonic wall thickening and stranding of the transverse, descending and sigmoid colon. Infectious work-up was unrevealing. A flexible sigmoidoscopy showed discontinuous areas of ulcerated and necrotic mucosa with stigmata of recent bleeding from the rectum to the descending colon (Figure A and B). While a subset of biopsy fragments appeared edematous but near normal, others had ischemic glandular attenuation, stromal hemorrhage, and surface ulceration with occasional pseudomembrane formation consistent with HSV colitis. Immunosuppressants were held and she completed a two-week course of valacyclovir 1 gram 3 times daily with resolution of her GI symptoms.
Discussion: We present a unique case of HSV colitis associated with disseminated cutaneous HSV infection in an immunosuppressed patient. Immunosuppression increases the risk for dissemination of HSV, however colonic involvement is rare. Endoscopic and pathologic confirmation is essential. Management involves withholding immunosuppressive therapy if possible and initiating antivirals promptly. The preferred therapy is acyclovir or valacyclovir for a two-week course. The early recognition of HSV colitis in immunocompromised patients is crucial to reach an early diagnosis, evaluate the need to hold immunotherapy, and to ensure timely and successful treatment to prevent fatal outcomes.

Disclosures:
Jasmine Tidwell, MD, Minh Thu T. Nguyen, MD, Maryam Zenali, MD, Faripour Forouhar, MD, Campbell Stewart, MD, Roopjeet Bath, MD. P3142 - A Case of Herpes Simplex Virus Colitis in an Immunosuppressed Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
UConn Health, Farmington, CT
Introduction: Herpes simplex virus (HSV) is a common virus capable of pathologies ranging from cold sores to colitis. When the gastrointestinal tract is involved, it usually affects the esophagus, perineum, and rectum. We describe a rare case of disseminated cutaneous HSV infection with concomitant colonic involvement in an immunosuppressed patient.
Case Description/Methods: A 48-year-old woman with a past medical history of systemic lupus erythematous previously complicated by pericardial effusion and lupus nephritis, presented due to a progressive rash. Her medications included mycophenolate mofetil 1 gram twice a day, voclosporin 23.7 mg twice daily, and prednisone 20 mg daily. The rash developed 10 days prior to admission, starting on her left buttock, then spreading to the pubic region, labia majora and perianal region. Skin viral swabs were positive for HSV type 2, which was confirmed with a punch biopsy. She was subsequently started on antiviral therapy.
Her hospital course was complicated by acute onset of watery diarrhea with hematochezia and small blood clots. CT scan of the abdomen and pelvis revealed colonic wall thickening and stranding of the transverse, descending and sigmoid colon. Infectious work-up was unrevealing. A flexible sigmoidoscopy showed discontinuous areas of ulcerated and necrotic mucosa with stigmata of recent bleeding from the rectum to the descending colon (Figure A and B). While a subset of biopsy fragments appeared edematous but near normal, others had ischemic glandular attenuation, stromal hemorrhage, and surface ulceration with occasional pseudomembrane formation consistent with HSV colitis. Immunosuppressants were held and she completed a two-week course of valacyclovir 1 gram 3 times daily with resolution of her GI symptoms.
Discussion: We present a unique case of HSV colitis associated with disseminated cutaneous HSV infection in an immunosuppressed patient. Immunosuppression increases the risk for dissemination of HSV, however colonic involvement is rare. Endoscopic and pathologic confirmation is essential. Management involves withholding immunosuppressive therapy if possible and initiating antivirals promptly. The preferred therapy is acyclovir or valacyclovir for a two-week course. The early recognition of HSV colitis in immunocompromised patients is crucial to reach an early diagnosis, evaluate the need to hold immunotherapy, and to ensure timely and successful treatment to prevent fatal outcomes.

Figure: Figure A – Flexible sigmoidoscopy showed deep ulcers and necrotic mucosa in the descending colon. Figure B – Flexible sigmoidoscopy showed deep ulcers and necrotic mucosa in the splenic flexure.
Disclosures:
Jasmine Tidwell indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Maryam Zenali indicated no relevant financial relationships.
Faripour Forouhar indicated no relevant financial relationships.
Campbell Stewart indicated no relevant financial relationships.
Roopjeet Bath indicated no relevant financial relationships.
Jasmine Tidwell, MD, Minh Thu T. Nguyen, MD, Maryam Zenali, MD, Faripour Forouhar, MD, Campbell Stewart, MD, Roopjeet Bath, MD. P3142 - A Case of Herpes Simplex Virus Colitis in an Immunosuppressed Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

