Tuesday Poster Session
Category: Small Intestine
P4143 - A Case of Eosinophilic Gastrointestinal Disease Presenting as Eosinophilic Ascites
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Savannah Danell, MD
Madigan Army Medical Center
Tacoma, WA
Presenting Author(s)
Savannah Danell, MD1, Robert Spiller, DO2
1Madigan Army Medical Center, Tacoma, WA; 2Walter Reed National Military Medical Center, Bethesda, MD
The views expressed are those of the author(s) and do not reflect the official policy of the Department of the Army, the Department of Defense or the U.S. Government.
Introduction: Eosinophilic gastrointestinal disease (EGID) is becoming more prevalent and must be considered in patients with nonspecific GI symptoms and peripheral eosinophilia. While atypical, patients may also present with eosinophilic ascites. We present a patient with multiple healthcare visits who was ultimately diagnosed with EGID.
Case Description/Methods: A 24-year-old female presented with three weeks of nausea, vomiting, diarrhea, and abdominal distension with an admission one week prior for similar symptoms. Previous workup was significant for abdominal computed tomography (CT) showing thickening of the duodenum and jejunum as well as ascites. Labs during that admission were most notable for an absolute eosinophil count (AEC) of 2500 and C-reactive protein of 33 mg/L. Complete metabolic panel, tryptase, stool ova and parasites, Strongyloides, enteric pathogen panel and fecal calprotectin were negative/normal. She was treated supportively for a presumed infectious enteritis, experienced slight improvement of symptoms, and was discharged after one day. The patient then had symptom relapse and a repeat CT scan showed significant bowel wall thickening which had progressed to involve the distal small bowel as well as the ascending and descending colon and diffuse ascites. Laboratory tests again noted an elevated AEC of 1600. A diagnostic paracentesis showed low serum-albumin ascites gradient (< 1.1) with eosinophils of 1,254. She underwent an esophagogastroduodenoscopy and colonoscopy. Duodenal, ileal and ascending/sigmoid colon biopsies revealed markedly increased eosinophils. Duodenal biopsies noted infiltration to the submucosa. Given her peripheral eosinophilia, eosinophilic ascites and marked elevation of eosinophils within the small and large bowel, she was diagnosed with EGID and subsequently started on dexamethasone with significant symptomatic improvement and normalization of her peripheral eosinophilia.
Discussion: We present a patient with nonspecific GI symptoms who was found to have eosinophilic infiltration to the duodenal submucosa, along with a marked increase in eosinophils to the ileum and colon. We propose that the infiltration led to her findings of eosinophilic ascites, which is an uncommon presentation of a relatively rare diagnosis, EGID. We also suggest that symptoms of EGID, including ascites, can be responsive to steroid therapy.

Disclosures:
Savannah Danell, MD1, Robert Spiller, DO2. P4143 - A Case of Eosinophilic Gastrointestinal Disease Presenting as Eosinophilic Ascites, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Madigan Army Medical Center, Tacoma, WA; 2Walter Reed National Military Medical Center, Bethesda, MD
The views expressed are those of the author(s) and do not reflect the official policy of the Department of the Army, the Department of Defense or the U.S. Government.
Introduction: Eosinophilic gastrointestinal disease (EGID) is becoming more prevalent and must be considered in patients with nonspecific GI symptoms and peripheral eosinophilia. While atypical, patients may also present with eosinophilic ascites. We present a patient with multiple healthcare visits who was ultimately diagnosed with EGID.
Case Description/Methods: A 24-year-old female presented with three weeks of nausea, vomiting, diarrhea, and abdominal distension with an admission one week prior for similar symptoms. Previous workup was significant for abdominal computed tomography (CT) showing thickening of the duodenum and jejunum as well as ascites. Labs during that admission were most notable for an absolute eosinophil count (AEC) of 2500 and C-reactive protein of 33 mg/L. Complete metabolic panel, tryptase, stool ova and parasites, Strongyloides, enteric pathogen panel and fecal calprotectin were negative/normal. She was treated supportively for a presumed infectious enteritis, experienced slight improvement of symptoms, and was discharged after one day. The patient then had symptom relapse and a repeat CT scan showed significant bowel wall thickening which had progressed to involve the distal small bowel as well as the ascending and descending colon and diffuse ascites. Laboratory tests again noted an elevated AEC of 1600. A diagnostic paracentesis showed low serum-albumin ascites gradient (< 1.1) with eosinophils of 1,254. She underwent an esophagogastroduodenoscopy and colonoscopy. Duodenal, ileal and ascending/sigmoid colon biopsies revealed markedly increased eosinophils. Duodenal biopsies noted infiltration to the submucosa. Given her peripheral eosinophilia, eosinophilic ascites and marked elevation of eosinophils within the small and large bowel, she was diagnosed with EGID and subsequently started on dexamethasone with significant symptomatic improvement and normalization of her peripheral eosinophilia.
Discussion: We present a patient with nonspecific GI symptoms who was found to have eosinophilic infiltration to the duodenal submucosa, along with a marked increase in eosinophils to the ileum and colon. We propose that the infiltration led to her findings of eosinophilic ascites, which is an uncommon presentation of a relatively rare diagnosis, EGID. We also suggest that symptoms of EGID, including ascites, can be responsive to steroid therapy.

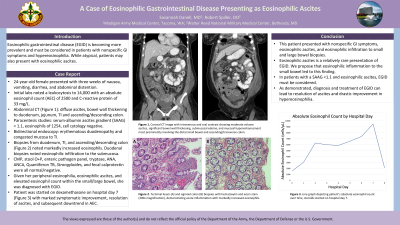
Figure: Coronal computed tomography image with intravenous and oral contrast showing moderate volume ascites, significant bowel wall thickening, submucosal edema, and mucosal hyperenhancement most prominently involving the distal small bowel and ascending/transverse colon (A,B). Terminal ileum (C) and sigmoid colon (D) biopsies with hematoxylin and eosin stain (200x magnification), demonstrating acute inflammation with markedly increased eosinophils.
Disclosures:
Savannah Danell indicated no relevant financial relationships.
Robert Spiller indicated no relevant financial relationships.
Savannah Danell, MD1, Robert Spiller, DO2. P4143 - A Case of Eosinophilic Gastrointestinal Disease Presenting as Eosinophilic Ascites, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
