Tuesday Poster Session
Category: Small Intestine
P4145 - The Peeking Brunner’s: A Rare Case of Prolapsed Giant Brunner’s Gland Hamartoma Through the Gastric Pylorus with No Clinically Overt Gastric Outlet Obstruction
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Philip Oppong-Twene, MD, MPH
Howard University Hospital
Washington, DC
Presenting Author(s)
Philip Oppong-Twene, MD, MPH1, Suryanarayana Reddy Challa, MD1, Justice Arhinful, MD1, Sabesan Balasinkam, MD1, Babak Shokrani, MD1, Angesom Kibreab, MD2
1Howard University Hospital, Washington, DC; 2Howard University Hospital, Washington, WA
Introduction: Hamartomas of the Brunner’s gland are rare polypoid masses in the proximal duodenum. They account for about 5% of all duodenal masses. Giant Brunner’s gland hamartomas more than 10 cm are extremely rare, and can be symptomatic, presenting with gastrointestinal obstruction or Iron deficiency anemia (IDA).
Case Description/Methods: A 72-year-old male with medical history of hypertension was referred by his hematologist for diagnostic Esophagogastroduodenoscopy (EGD) and Colonoscopy for IDA. He reported 12 lbs unintentional weight loss within 2 months and fatigue. He denied abdominal pain, nausea, vomiting, overt gastrointestinal blood loss, anti-coagulation and NSAIDS use.
Physical examination revealed mild conjunctival pallor. Cardiorespiratory and abdominal examination were normal.
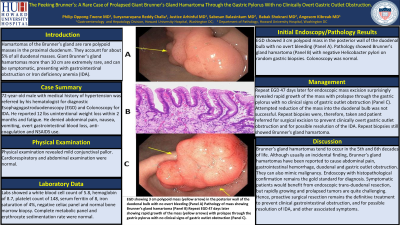
Labs showed a white blood cell count of 5.8, hemoglobin of 8.7, platelet count of 148, serum ferritin of 8, iron saturation of 4%, negative celiac panel and normal bone marrow biopsy. Complete metabolic panel and erythrocyte sedimentation rate were normal. EGD showed 3 cm polypoid mass in the posterior wall of the duodenal bulb with no overt bleeding (Panel A). Pathology showed Brunner’s gland hamartoma (Panel B) with negative Helicobacter pylori on random gastric biopsies. Colonoscopy was normal. Repeat EGD 47 days later for endoscopic mass excision surprisingly revealed rapid growth of the mass with prolapse through the gastric pylorus with no clinical signs of gastric outlet obstruction (Panel C). Attempted reduction of the mass into the duodenal bulb was not successful. Repeat biopsies were, therefore, taken and patient referred for surgical excision to prevent clinically overt gastric outlet obstruction and for possible resolution of the IDA. Repeat biopsies still showed Brunner's gland hamartoma.
Discussion: Brunner’s gland hamartomas tend to occur in the 5th and 6th decades of life. Although usually an incidental finding, Brunner’s gland hamartomas have been reported to cause abdominal pain, gastrointestinal hemorrhage, duodenal and gastric outlet obstruction. They can also mimic malignancy. Endoscopy with histopathological confirmation remains the gold standard for diagnosis.
Symptomatic patients would be benefit from endoscopic trans-duodenal resection, but rapidly growing and prolapsed tumors are quite challenging. Hence, proactive surgical resection remains the definitive treatment to prevent clinical gastrointestinal obstruction, and for possible resolution of IDA, and other associated symptoms.

Disclosures:
Philip Oppong-Twene, MD, MPH1, Suryanarayana Reddy Challa, MD1, Justice Arhinful, MD1, Sabesan Balasinkam, MD1, Babak Shokrani, MD1, Angesom Kibreab, MD2. P4145 - The Peeking Brunner’s: A Rare Case of Prolapsed Giant Brunner’s Gland Hamartoma Through the Gastric Pylorus with No Clinically Overt Gastric Outlet Obstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Howard University Hospital, Washington, DC; 2Howard University Hospital, Washington, WA
Introduction: Hamartomas of the Brunner’s gland are rare polypoid masses in the proximal duodenum. They account for about 5% of all duodenal masses. Giant Brunner’s gland hamartomas more than 10 cm are extremely rare, and can be symptomatic, presenting with gastrointestinal obstruction or Iron deficiency anemia (IDA).
Case Description/Methods: A 72-year-old male with medical history of hypertension was referred by his hematologist for diagnostic Esophagogastroduodenoscopy (EGD) and Colonoscopy for IDA. He reported 12 lbs unintentional weight loss within 2 months and fatigue. He denied abdominal pain, nausea, vomiting, overt gastrointestinal blood loss, anti-coagulation and NSAIDS use.
Physical examination revealed mild conjunctival pallor. Cardiorespiratory and abdominal examination were normal.
Labs showed a white blood cell count of 5.8, hemoglobin of 8.7, platelet count of 148, serum ferritin of 8, iron saturation of 4%, negative celiac panel and normal bone marrow biopsy. Complete metabolic panel and erythrocyte sedimentation rate were normal. EGD showed 3 cm polypoid mass in the posterior wall of the duodenal bulb with no overt bleeding (Panel A). Pathology showed Brunner’s gland hamartoma (Panel B) with negative Helicobacter pylori on random gastric biopsies. Colonoscopy was normal. Repeat EGD 47 days later for endoscopic mass excision surprisingly revealed rapid growth of the mass with prolapse through the gastric pylorus with no clinical signs of gastric outlet obstruction (Panel C). Attempted reduction of the mass into the duodenal bulb was not successful. Repeat biopsies were, therefore, taken and patient referred for surgical excision to prevent clinically overt gastric outlet obstruction and for possible resolution of the IDA. Repeat biopsies still showed Brunner's gland hamartoma.
Discussion: Brunner’s gland hamartomas tend to occur in the 5th and 6th decades of life. Although usually an incidental finding, Brunner’s gland hamartomas have been reported to cause abdominal pain, gastrointestinal hemorrhage, duodenal and gastric outlet obstruction. They can also mimic malignancy. Endoscopy with histopathological confirmation remains the gold standard for diagnosis.
Symptomatic patients would be benefit from endoscopic trans-duodenal resection, but rapidly growing and prolapsed tumors are quite challenging. Hence, proactive surgical resection remains the definitive treatment to prevent clinical gastrointestinal obstruction, and for possible resolution of IDA, and other associated symptoms.

Figure: EGD showing 3 cm polypoid mass (yellow arrow) in the posterior wall of the duodenal bulb with no overt bleeding (Panel A) Pathology of mass showing Brunner’s gland hamartoma (Panel B) Repeat EGD 47 days later showing rapid growth of the mass (yellow arrows) with prolapse through the gastric pylorus with no clinical signs of gastric outlet obstruction (Panel C).
Disclosures:
Philip Oppong-Twene indicated no relevant financial relationships.
Suryanarayana Reddy Challa indicated no relevant financial relationships.
Justice Arhinful indicated no relevant financial relationships.
Sabesan Balasinkam indicated no relevant financial relationships.
Babak Shokrani indicated no relevant financial relationships.
Angesom Kibreab indicated no relevant financial relationships.
Philip Oppong-Twene, MD, MPH1, Suryanarayana Reddy Challa, MD1, Justice Arhinful, MD1, Sabesan Balasinkam, MD1, Babak Shokrani, MD1, Angesom Kibreab, MD2. P4145 - The Peeking Brunner’s: A Rare Case of Prolapsed Giant Brunner’s Gland Hamartoma Through the Gastric Pylorus with No Clinically Overt Gastric Outlet Obstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
