Tuesday Poster Session
Category: Small Intestine
P4147 - IgA Vasculitis Associated With COVID-19 Presenting as Acute Terminal Ileitis and Acute Appendicitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- ML
Maunoo Lee, MD
Naval Medical Center
San Diego, CA
Presenting Author(s)
Maunoo Lee, MD, Jonathan Cho, MD, PhD, Jeremy Drenckhahn, MD, Brett Sadowski, MD
Naval Medical Center, San Diego, CA
Introduction: IgA vasculitis uncommonly affects adults and may present with intermittent abdominal pain, arthralgia, purpura, and kidney disease, mimicking symptoms associated with inflammatory bowel disease and appendicitis if there is no skin and renal involvement.
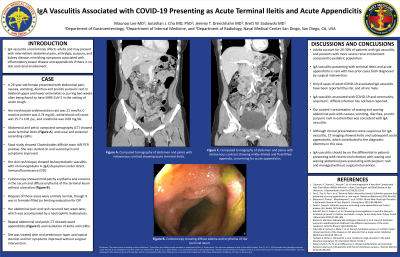
Case Description/Methods: A 26-year-old female presented with abdominal pain, nausea, vomiting, diarrhea and pruritic purpuric rash in bilateral upper and lower extremities occurring two weeks after being found to have SARS-CoV-2 in the setting of acute cough... Her erythrocyte sedimentation rate was 21 mm/hr, C-reactive protein was 4.74 mg/dL, white blood cell count was 15.7 x 103 /μL, and creatinine was 0.68 mg/dL. Abdominal and pelvic computed tomography (CT) showed acute terminal ileitis, and cecal and proximal ascending colitis. Stool study showed Clostridioides difficile toxin A/B PCR positive. She was started on oral vancomycin and symptoms improved. Her skin rash biopsy showed leukocytoclastic vasculitis with immunoglobulin A (IgA) deposition under direct immunofluorescence (DIF). Colonoscopy showed mild patchy erythema and erosions in the cecum and diffuse erythema of the terminal ileum without ulceration. Biopsies of those areas were entirely normal, though it was in formalin-filled jar limiting evaluation for DIF. Her abdominal pain and rash recurred two week later, which was accompanied by a neutrophilic leukocytosis. Repeat abdominal and pelvic CT showed acute appendicitis and resolution of ileitis and colitis. She was treated with oral prednisone taper and topical steroids and her symptoms improved without surgical intervention.
Discussion: IgA vasculitis presenting with terminal ileitis and acute appendicitis is rare with two prior cases both diagnosed by surgical intervention. Only 8 cases of adult COVID-19 associated IgA vasculitis have been reported thus far, and all are male. Our patient’s presentation of waxing and waning abdominal pain with nausea, vomiting, diarrhea, pruritic purpuric rash in extremities was consistent with IgA vasculitis. Although clinical presentations were suspicious for IgA vasculitis, CT imaging showed ileitis and subsequent acute appendicitis, which contributed to the diagnostic dilemma in this case. IgA vasculitis should be on the differential in patients presenting with recent viral infection with waxing and waning abdominal pain associating with purpuric rash and managed without surgical intervention.

Disclosures:
Maunoo Lee, MD, Jonathan Cho, MD, PhD, Jeremy Drenckhahn, MD, Brett Sadowski, MD. P4147 - IgA Vasculitis Associated With COVID-19 Presenting as Acute Terminal Ileitis and Acute Appendicitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Naval Medical Center, San Diego, CA
Introduction: IgA vasculitis uncommonly affects adults and may present with intermittent abdominal pain, arthralgia, purpura, and kidney disease, mimicking symptoms associated with inflammatory bowel disease and appendicitis if there is no skin and renal involvement.
Case Description/Methods: A 26-year-old female presented with abdominal pain, nausea, vomiting, diarrhea and pruritic purpuric rash in bilateral upper and lower extremities occurring two weeks after being found to have SARS-CoV-2 in the setting of acute cough... Her erythrocyte sedimentation rate was 21 mm/hr, C-reactive protein was 4.74 mg/dL, white blood cell count was 15.7 x 103 /μL, and creatinine was 0.68 mg/dL. Abdominal and pelvic computed tomography (CT) showed acute terminal ileitis, and cecal and proximal ascending colitis. Stool study showed Clostridioides difficile toxin A/B PCR positive. She was started on oral vancomycin and symptoms improved. Her skin rash biopsy showed leukocytoclastic vasculitis with immunoglobulin A (IgA) deposition under direct immunofluorescence (DIF). Colonoscopy showed mild patchy erythema and erosions in the cecum and diffuse erythema of the terminal ileum without ulceration. Biopsies of those areas were entirely normal, though it was in formalin-filled jar limiting evaluation for DIF. Her abdominal pain and rash recurred two week later, which was accompanied by a neutrophilic leukocytosis. Repeat abdominal and pelvic CT showed acute appendicitis and resolution of ileitis and colitis. She was treated with oral prednisone taper and topical steroids and her symptoms improved without surgical intervention.
Discussion: IgA vasculitis presenting with terminal ileitis and acute appendicitis is rare with two prior cases both diagnosed by surgical intervention. Only 8 cases of adult COVID-19 associated IgA vasculitis have been reported thus far, and all are male. Our patient’s presentation of waxing and waning abdominal pain with nausea, vomiting, diarrhea, pruritic purpuric rash in extremities was consistent with IgA vasculitis. Although clinical presentations were suspicious for IgA vasculitis, CT imaging showed ileitis and subsequent acute appendicitis, which contributed to the diagnostic dilemma in this case. IgA vasculitis should be on the differential in patients presenting with recent viral infection with waxing and waning abdominal pain associating with purpuric rash and managed without surgical intervention.

Figure: Figure 1. IgA vasculitis presenting as acute terminal ileitis and acute appendicitis. a. Computed tomography of abdomen and pelvis with intravenous contrast showing acute terminal ileitis. b. Colonoscopy showing diffuse edema and erythema of the terminal ileum. c. Computed tomography of abdomen and pelvis with intravenous contrast showing mildly dilated and fluid-filled appendix, concerning for acute appendicitis.
Disclosures:
Maunoo Lee indicated no relevant financial relationships.
Jonathan Cho indicated no relevant financial relationships.
Jeremy Drenckhahn indicated no relevant financial relationships.
Brett Sadowski indicated no relevant financial relationships.
Maunoo Lee, MD, Jonathan Cho, MD, PhD, Jeremy Drenckhahn, MD, Brett Sadowski, MD. P4147 - IgA Vasculitis Associated With COVID-19 Presenting as Acute Terminal Ileitis and Acute Appendicitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
